16.5 Right ventricular infarction
Right ventricular infarction occurs in 30-50% of patients with inferior myocardial infarction, especially when the proximal right coronary artery is involved. Fortunately, right ventricular function returns to normal in most cases. Blood supply to the right ventricle is achieved by several means: the posterior descending branch supplies the posterior and inferior walls of the right ventricle, marginal branches of the RCA supply the lateral wall and the conus branch, as well as the moderator branch artery the anterior wall. In addition, thebesian veins and oxygen flowing directly from the cavity supply the right ventricular myocardium. As the right ventricle receives its blood supply by several routes and needs less oxygen, it is generally less susceptible to ischemic myocardial damage.
Patients with right heart infarction have a poor prognosis.Right ventricular infarction usually leads to right heart dilatation. RV infarction should be suspected in all patients with inferior infarctions and a dilated right ventricle. This applies to the presence of tricuspid regurgitation (as a plausible reason for RV dilatation) as well, because TR could be a secondary phenomenon.
It is important to look at the regional wall motion of the right ventricle on a four-chamber view as well as on atypical views because these demonstrate the anterior and posterior wall.
Most right ventricular infarctions are located in the posterior wall and the posterior septum.Video Platform
Video Management
Video Solutions
Video Player RCA occlusion: the free lateral wall of the right ventricle is akinetic.
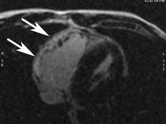
Aside from visual assessment of RV myocardial function, one may use tissue Doppler or myocardial strain imaging to detect segments with reduced contractility. However, these findings may be difficult to interpret and also inferior to magnetic resonance imaging. The latter may be used to detect myocardial necrosis.
As RV infarctions impair right ventricular function, one will also observe a reduction in right ventricular stroke volume (low-velocity time integral across the pulmonary valve). The size of the right atrium may be increased due to elevated right atrial pressure or even right atrial ischemic involvement. In addition, one may anticipate an enlarged vena cava inferior with little or no respiratory variation.
Patients with pulmonary embolism and right heart infarction share the same features and may therefore be difficult to distinguish from each other.16.6 Arrhythmogenic right ventricular dysplasia (ARVD)
Arrhythmogenic right ventricular dysplasia is a genetic disease which leads to replacement of the myocardium with adipose or fibroadipose tissue. Although the right ventricle is most commonly involved, the condition may involve the left ventricle as well. Infiltration is most commonly located in the apical and infundibular portions of the right ventricle. Patients usually present with symptoms of arrhythmias that arise from the right ventricle. The arrhythmia may be life threatening and may lead to syncope as well as sudden cardiac death. It accounts for 15-20% of sudden cardiac deaths in young persons. Echocardiography plays an important role in the diagnosis of this disease. The following features may be found:
- Right ventricular dilatation and hypokinesia
- Isolated right ventricular outflow tract dilatation
- End-diastolic aneurysms
- Increased reflectivity of the moderator band
- Akinesia or dyskinesia of the inferobasal and apical right ventricular segments
- Prominent apical trabeculae
- Thin and hyperreflective right ventricular wall
Video Platform
Video Management
Video Solutions
Video Player Dilatation of the RV outflow tract in ARVD
Video Platform
Video Management
Video Solutions
Video Player Dilated right ventricle in ARVD
Video Platform
Video Management
Video Solutions
Video Player Prominent apical trabecula in ARVD
Despite the numerous symptoms and conditions that may be present, the sensitivity of the procedure for the detection of ARVD is lower than that of cardiac MRI. First, the findings may be quite subtle; second, the echocardiographic appearance may vary greatly; and third, MRI is superior in detecting fatty infiltration of the myocardium.
Recent studies suggest that right ventricular strain imaging using tissue Doppler as well as speckle tracking helps to detect regional functional abnormalities in patients with genetically confirmed and subtle forms of ARVD.
The diagnosis cannot be established by echocardiography alone; other criteria must also be present (i.e. ECG, family history, genetic testing for RV arrhythmia).