Occluded TIPS shunt
Case Presentation
35-year-old male, with a history of hepatic cirrhosis, ascites and a positive HbsAg, who underwent TIPS stenting. His ascites improved post stenting. Now 2 months post stent, he complains of increasing abdominal girth.
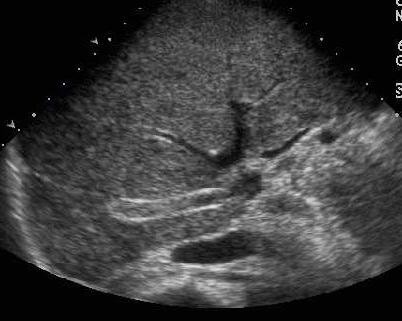 Caption: Transverse sonogram of the liver. | Description: Transverse section through the liver at the level of the hepatic veins, showing 2 curvilinear, parallel, echogenic lines coursing through the vein, identified as the TIPS stent.
Caption: Transverse sonogram of the liver. | Description: Transverse section through the liver at the level of the hepatic veins, showing 2 curvilinear, parallel, echogenic lines coursing through the vein, identified as the TIPS stent.
First published on SonoWorld
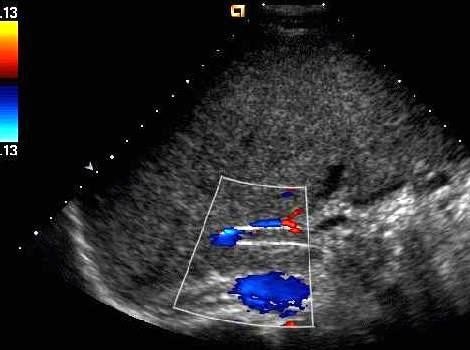 Caption: Color Doppler of the TIPS stent. | Description: Color Doppler study showing no color flow within the stent.
Caption: Color Doppler of the TIPS stent. | Description: Color Doppler study showing no color flow within the stent.
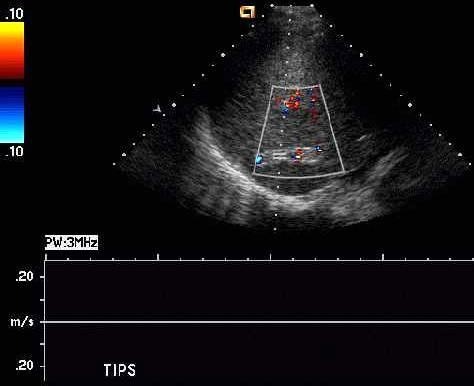 Caption: Spectral Doppler of the TIPS stent. | Description: Spectral Doppler study showing no flow in the central portion of the stent.
Caption: Spectral Doppler of the TIPS stent. | Description: Spectral Doppler study showing no flow in the central portion of the stent.
 Caption: Spectral Doppler of the TIPS stent. | Description: No recordable flow was noted through the peripheral part of the TIPS stent.
Caption: Spectral Doppler of the TIPS stent. | Description: No recordable flow was noted through the peripheral part of the TIPS stent.
Differential Diagnosis
Occluded TIPS shunt.
Final Diagnosis
Occluded TIPS shunt.
Discussion
TIPS [transjugular intrahepatic portosystemic shunt] is a percutaneously created shunt, aimed at reducing the portal pressure. The procedure involves placement of a stent, which spans the low- pressure intrahepatic and the high-pressure portal veins within the liver parenchyma. A catheter is manipulated through the right jugular vein [usually], through the right atrium, IVC and into the right hepatic vein. A needle is passed puncturing the hepatic vein wall, through the parenchyma into one of the branches of the portal vein. The track along the communication between hepatic vein and portal vein is then dilated and an expandable stent is deployed to keep the track open. This communication allows free flow of blood from the portal to the systemic circulation, thereby reducing the portal pressure. It also reduces the risk of life threatening variceal bleeds and ascites.
Portal hypertension is described as portal pressure greater than 12mm Hg. The current indications that have been accepted for TIPS, from the available data are:
- Acute or recurrent severe variceal bleeding refractory to endoscopic or medical treatment.
- Hepatic pleural effusion.
- Refractory ascites.
- Budd – Chiari syndrome.
The contraindications for this procedure include –
- Severe pre-existing hepatic encephalopathy.
- Cardiac failure.
- Fulminant hepatic failure.
TIPS complications are quite common, the most important of which are stenosis and blocked shunt. Hence follow up scanning is very important. Ultrasound with color Doppler imaging is one of the most cost effective modalities available to assess the adequacy of the shunt. A routine baseline scan should be done, which includes evaluation of the stent, quantifying ascites and identifying any hematomas or intraperitoneal bleeds. Gray scale imaging shows the stent as two echogenic curvilinear lines. The shunt diameter can be measured easily, but a curved TIPS may give the erroneous appearance of stenosis. One must remember that hepatofugal flow in the portal system is almost always abnormal. Patients experiencing increased portal venous pressure have a reversal of flow in the portal system (changing from the normal hepatopetal [toward the liver], to hepatofugal [away from the liver]). With a normally functioning shunt the flow direction of the entire portal system is toward the portal end of stent [flow in the main portal vein becomes hepatopetal and in the intraparenchymal branches of portal vein is variable]. The stent shows complete wall-to-wall filling with color.
Stenosis or a blocked stent is a common complication, the pathogenesis of which is based on a complex process of intimal hyperplasia. The literature is controversial with respect to the normal range of velocities within the shunt using Doppler ultrasound. Some use 90-190 cm/sec as the normal range. It is important to be aware of the fact that deep and sustained inspiration will result in a decrease in the peak velocity by 22 cm/second on an average, when compared to the velocity during quiet respiration. Hence respiratory variability should be kept in mind, while scanning. The reported Doppler criteria to recognize a dysfunctioning shunt are based on multiple velocity changes, temporal change criteria and flow direction change criteria:
a) Maximum velocity in the portal third of the shunt less than or equal to 50cm/s.
b) Maximum intrashunt velocity of less than 50-60 cm/second.
c) Peak intrashunt velocity greater than or equal to 250 cm/second.
d) Maximum portal vein velocity was less than or equal to two thirds (66.7%) of the baseline value.
e) A temporal change (increase or decrease) of greater than 50 cm/second in the peak velocity of the shunt from the base line study.
f) Hepatofugal flow in main portal vein or extrahepatic portal venous tributaries.
g) The right and left branches of portal vein show variable flow, depending on the site of placement of the TIPS stent.
If no flow is detected in the shunt, and the flow velocity and the direction of portal vein is the same as prior to the procedure, a blocked stent is to be considered. Early recognition of this complication can aid in either recanalization or stent replacement.
Follow Up
Unsuccessful TIPS revision attempted, via selective catheterization and instillation of contrast into the hepatic vein containing the central part of the stent. Presence of a thrombus was noted within and adjacent to the stent.
Case References
1. Chong WK, Malisch TA, Mazer MJ, Lind CD, Worrell JA, Richards WO: Transjugular intrahepatic portosystemic shunt: US assessment with maximum flow velocity. Radiology 1993; 189:789-793.
2. Foshager MC, Ferral H, et al: Colour Doppler sonography of transjugular intrahepatic portosystemic shunts (TIPS). AJR 1994; 163:105-111.
3. Dodd GD, Zajko AB, Orons PD, Martin MS, Eichner LS, Santaguida LA: Detection of transjugular intrahepatic portosystemic shunt dysfunction: value of duplex Doppler sonography. AJR 1995; 164:1119-1124.
4. J. Zizka, P. Eliás, A. Krajina, A. Michl, et al: Value of Doppler Sonography in Revealing Transjugular Intrahepatic Portosystemic Shunt Malfunction: A 5-Year Experience in 216 Patients. AJR 2000; 175(1): 141 - 148.
5. R. H. Wachsberg, P. Bahramipour, C. T. Sofocleous, and A. Barone.:Hepatofugal Flow in the Portal Venous System: Pathophysiology, Imaging Findings, and Diagnostic Pitfalls. RadioGraphics, January 1, 2002; 22(1): 123 - 140.

