7. Imaging the vertebral arteries
/* .lity-iframe-container iframe { background: #fff !important; } */ .articles__categories nav { display: none !important; } .sonopl-book__aside .articles__categories { background: #f5f5f5; } .sonopl-article th, .sonopl-article td { color: black; text-align: left; } function advagg_mod_1() { // Count how many times this function is called. advagg_mod_1.count = ++advagg_mod_1.count || 1; try { if (advagg_mod_1.count <= 40) { var getClass = document.querySelectorAll(".articles__categories"); var a = document.createElement('a'); var linkText = document.createTextNode("Get Carotid MC Free Lectures"); a.appendChild(linkText); a.title = "newsletter"; a.href = "/overlay/forms/cu_mc/16618"; a.setAttribute("class", "sonopl-button sonopl-button--default"); a.setAttribute("data-lity", ""); a.style = "line-height: 1.2;margin-top: 25px;padding: 15px;width: 100%;"; for(var ix = 0; ix < getClass.length; ix++) { getClass[ix].appendChild(a) } // Set this to 100 so that this function only runs once. advagg_mod_1.count = 100; } } catch(e) { if (advagg_mod_1.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_1, 250); } } } function advagg_mod_1_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_1(); } else { window.setTimeout(advagg_mod_1_check, 250); } } advagg_mod_1_check();
Imaging of the vertebral arteries is part of a standard extra-cranial cerebrovascular ultrasound duplex scan. The vertebral arteries are smaller, located more distal from the transducer and partially “hidden” behind the bony structures of the vertebrae. Therefore they are more difficult to image. Despite these limitations it is possible to visualize and obtain flow information in the vertebral arteries in the vast majority of patients. To achieve optimal results it is important to understand the topography of the vertebral arteries and to use all possible ultrasound modalities (B Mode, color Doppler and spectral Doppler) and practice. It is important to recognize that Magnetic Resonance Angiography, CT Angiography and Digital Subtraction Angiography are superior (sensitive) to ultrasound in the detection of vertebral artery pathologies. In contrast extra-cranial ultrasound has numerous advantages:
- It is less complex
- It carries no risk
- It is more cost effective
- Can be applied bedside
- More available
- Provides hemodynamic information
7.1 What is the anatomy of the vertebral arteries
The vertebral arteries arise bilaterally from the subclavian artery they travel posterior to the carotid artery (in the back of the neck) cranially to enter the skull through the vertebral canal. Both vertebral arteries join to form the basilar artery.
Note: The left vertebral artery arises from the aorta in approximately 3-5% of patients
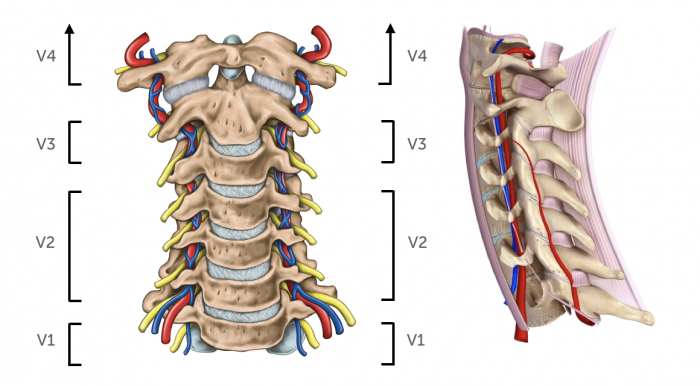 Vertebral artery anatomy. Left: segments of the vertebral arteries; Right: course of the vertebral artery and vein through the transverse processes of the vertebrae
Vertebral arteries - Topography
Segments
Origin
Subclavian artery
Origin is visible in 60-70%
Location
The vertebral arteries are posterior and lateral to common carotid artery
Can be imaged behind the carotid artery or from a more laterally angulated position (or by moving the transducer more lateral)
Course
Runs in the transverse foramen of the cervical vertebra. Enters the skull through the foramen magnum
Bony structures obscure the view. The vessels is interrupted on the US image. Tortuosity can be found (especially V1)
Vertebral artery anatomy. Left: segments of the vertebral arteries; Right: course of the vertebral artery and vein through the transverse processes of the vertebrae
Vertebral arteries - Topography
Segments
Origin
Subclavian artery
Origin is visible in 60-70%
Location
The vertebral arteries are posterior and lateral to common carotid artery
Can be imaged behind the carotid artery or from a more laterally angulated position (or by moving the transducer more lateral)
Course
Runs in the transverse foramen of the cervical vertebra. Enters the skull through the foramen magnum
Bony structures obscure the view. The vessels is interrupted on the US image. Tortuosity can be found (especially V1)
7.2 Which regions do the vertebral arteries supply?
The vertebral arteries supply blood to the cranial part of the spinal cord, the brainstem and the cerebellum as wall as the posterior part of the brain. A stroke (occlusion, embolizaton) of the vertebral artery will affect the posterior circulation of the brain. Approximately 20-25% of all strokes affect the vertebrobasilar system. Strokes of the large arteries of the posterior circulation will often be fatal or cause severe disability. Typical symptoms include: ataxia vertigo, nausea, slurred speech or double vision. The vertebral arteries also play an important role as a collateral pathway in the setting of a proximal subclavian artery occlusion / stenosis by providing blood to the arm (subclavian steal syndrome). The vertebral arteries / basilar artery as part of the circle of Willis can also provide collateral blood flow in the setting of carotid artery occlusion. Conversely, occlusion of the vertebral artery does not invariable cause a stroke. Possibly the vertebral circulation is also protected by collateral blood flow through ascending cervical branches.
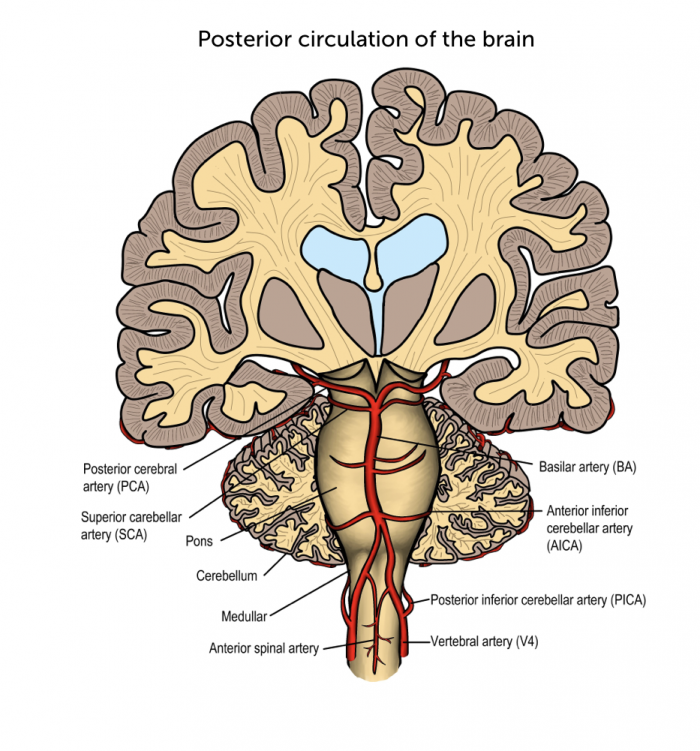 Posterior circulation. The posterior circulation of the brain receives blood from the vertebral arteries and is connected to the circle of Willis
Posterior circulation. The posterior circulation of the brain receives blood from the vertebral arteries and is connected to the circle of Willis
7.3 How can you find the vertebral arteries with ultrasound?
It can be challenging to visualize the vertebral arteries. Especially if they are small (hypoplastic) or occluded (no flow signal). Imaging of the vertebral arteries is more difficult in patients with “thick” short necks / obese patients. The vertebral artery is best visualized in a longitudinal view. Start by imaging the middle portion of the vertebral artery (V2) and then move caudally (to display the origin of the vertebral artery) and then more cranial to image the more distal portions of the vessel.
- Display the common carotid artery in a longitudinal view
- Slide laterally more posterior
- Angulate more posterior
- Display the vertebrae with the transverse processes (characterized by intermittent areas of shadowing) in between you will find the vertebral artery
Alternatively one can also use a more anterior transducer position imaging the vertebral arteries behind the common carotid artery.
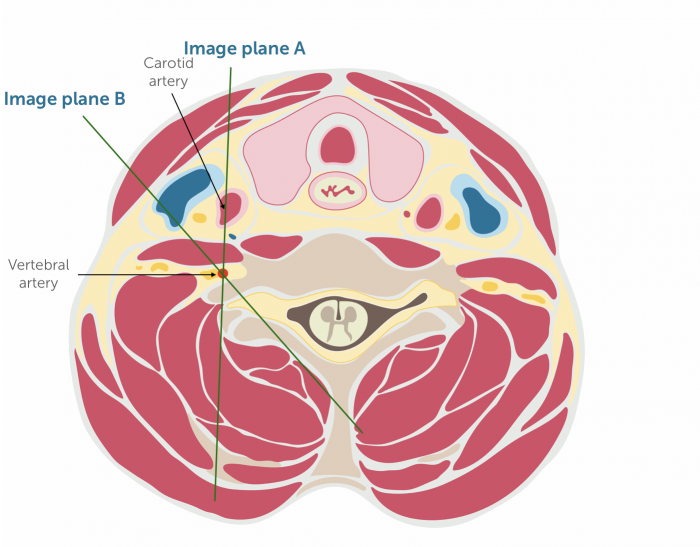 Va Imaging planes. Imaging planes to visualize the vertebral arteries. The vertebral arteries are posterior to the carotid arteries, You can chose an anterior (Image plane A) or more lateral approach (Image plane B)
Va Imaging planes. Imaging planes to visualize the vertebral arteries. The vertebral arteries are posterior to the carotid arteries, You can chose an anterior (Image plane A) or more lateral approach (Image plane B)
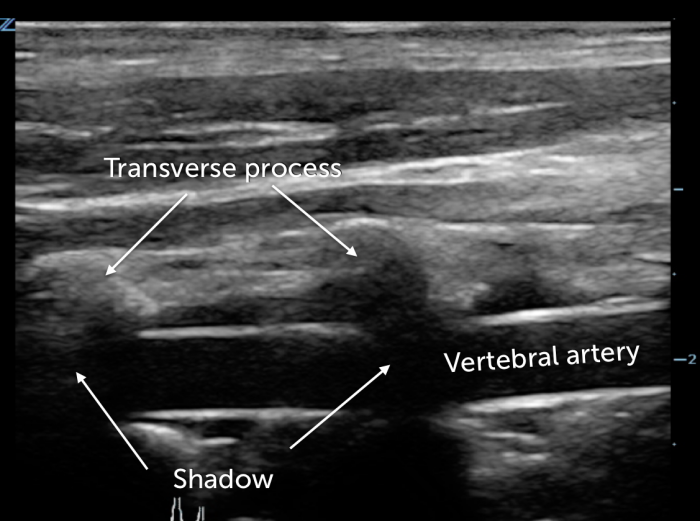 VA B Mode. Vertebral artery – B mode imaging. Visualization of the transverse processes with its characteristic posterior shadowing will guide you to the vertebral artery
VA B Mode. Vertebral artery – B mode imaging. Visualization of the transverse processes with its characteristic posterior shadowing will guide you to the vertebral artery
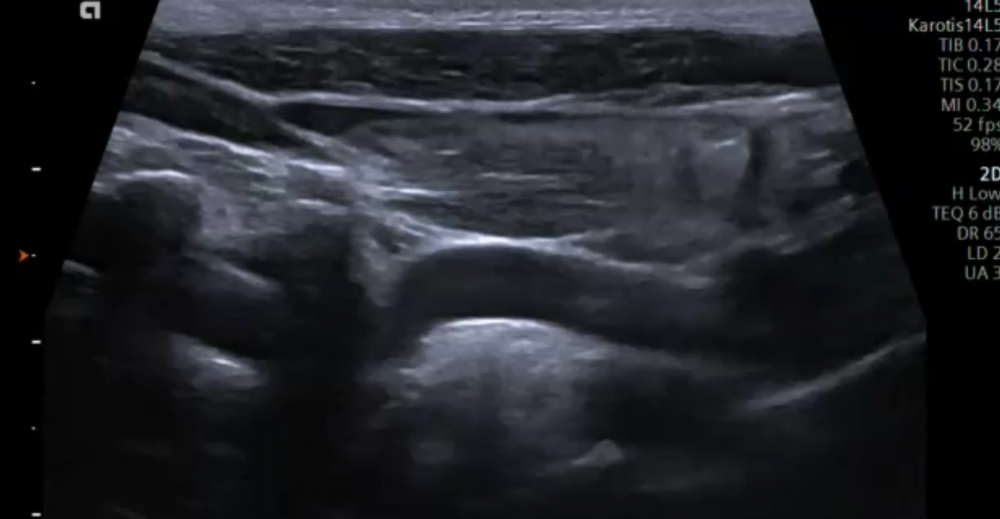 Va Loop. Ultrasound of the vertebral artery from its origin (subclavian artery – right of the image). Note the view is partially obscured by the transverse processes. Also note that the vertebral artery shows some degree of tortuosity.
Va Loop. Ultrasound of the vertebral artery from its origin (subclavian artery – right of the image). Note the view is partially obscured by the transverse processes. Also note that the vertebral artery shows some degree of tortuosity.
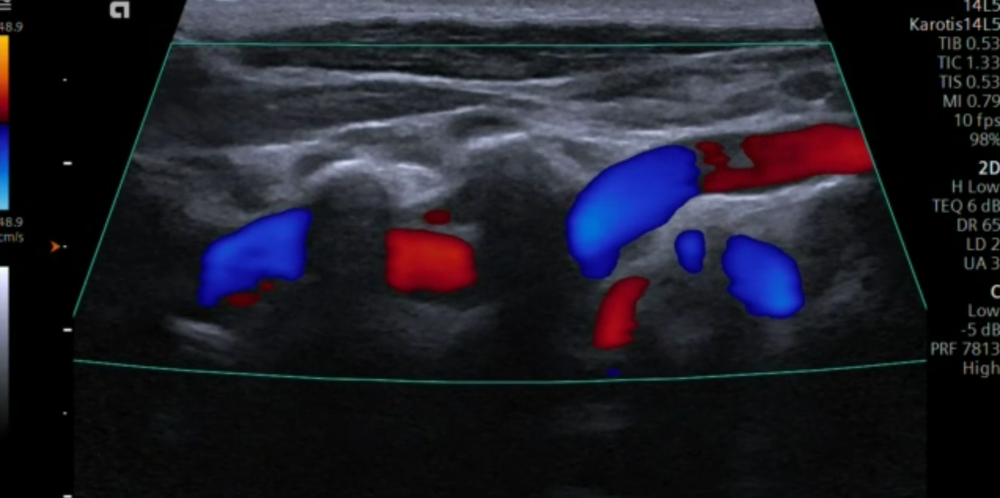 Va Loop_Color. Ultrasound of the vertebral artery. Note that the color changes from red to blue. This denotes a change in the orientation of the vessel due to its tortuosity
Va Loop_Color. Ultrasound of the vertebral artery. Note that the color changes from red to blue. This denotes a change in the orientation of the vessel due to its tortuosity
7.4 What is the normal size of vertebral arteries?
Normal size 3-5mm Hypoplasia < 2-3mm or side difference of > 1:1.7 (note in hypoplasia one can often find a larger vertebral artery on the contralateral side) Left vs. right The left is more commonly larger than the right Aplasia No vertebral artery present - uncommon - 1% of population Impact The posterior circulation is more vulnerable to ischemia in patients with vertebral artery hypoplasia
7.5 How do I use color Doppler in the assessment of the vertebral arteries?
Color Doppler is helpful to locate the vertebral artery. Make sure that you optimize the color Doppler box to the direction of flow. Color Doppler is also used to determine the direction of flow and to differentiate the artery from the vein. Areas of turbulent flow indicates a stenosis. The absence of a color flow signal within the vertebral artery indicates occlusion of the vertebral artery.
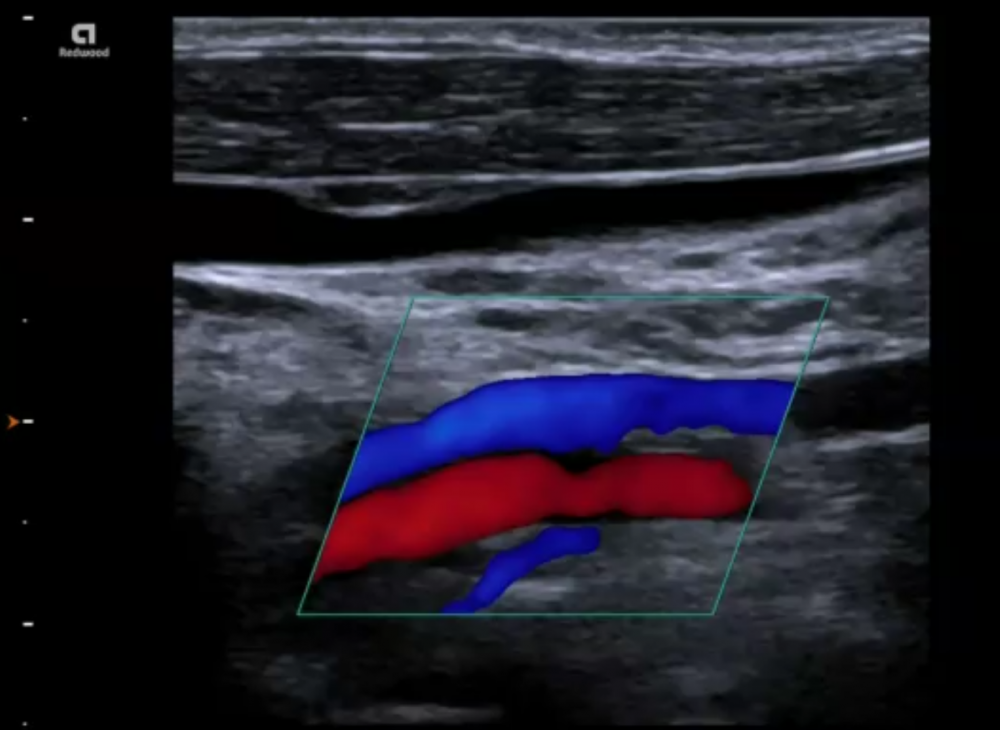 Va Artery + vein. Carotid Ultrasound imaging of the vertebral artery. Image displaying both the vertebral vein (blue) and the vertebral artery (red). The vein is proximal to the transducer.
Va Artery + vein. Carotid Ultrasound imaging of the vertebral artery. Image displaying both the vertebral vein (blue) and the vertebral artery (red). The vein is proximal to the transducer.
7.6 What is the role of spectral Doppler of the vertebral artery?
Spectral Doppler should routinely be performed during an ultrasound exam of the extracranial arteries. It allows you to:
- Differentiate the vertebral artery from the vertebral vein
- Determine the direction of flow
- Demonstrate flow within the vertebral artery
- Help to detect a vertebral artery stenosis
- Assess a dissection of the vertebral artery.
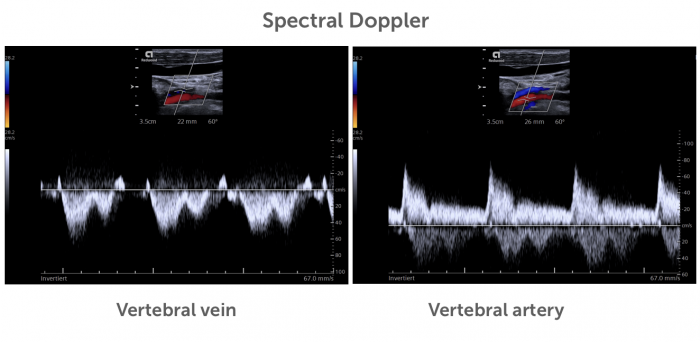 Spectral Doppler VA+VV. Spectral Doppler of the vertebral vein and artery. Note that the direction of flow differs (positive vs. negative flow). The pattern is also different. The vertebral artery typically shows systolic / diastolic (pulsatile) flow. Venous flow velocity is lower and more continuous.
Spectral Doppler VA+VV. Spectral Doppler of the vertebral vein and artery. Note that the direction of flow differs (positive vs. negative flow). The pattern is also different. The vertebral artery typically shows systolic / diastolic (pulsatile) flow. Venous flow velocity is lower and more continuous.
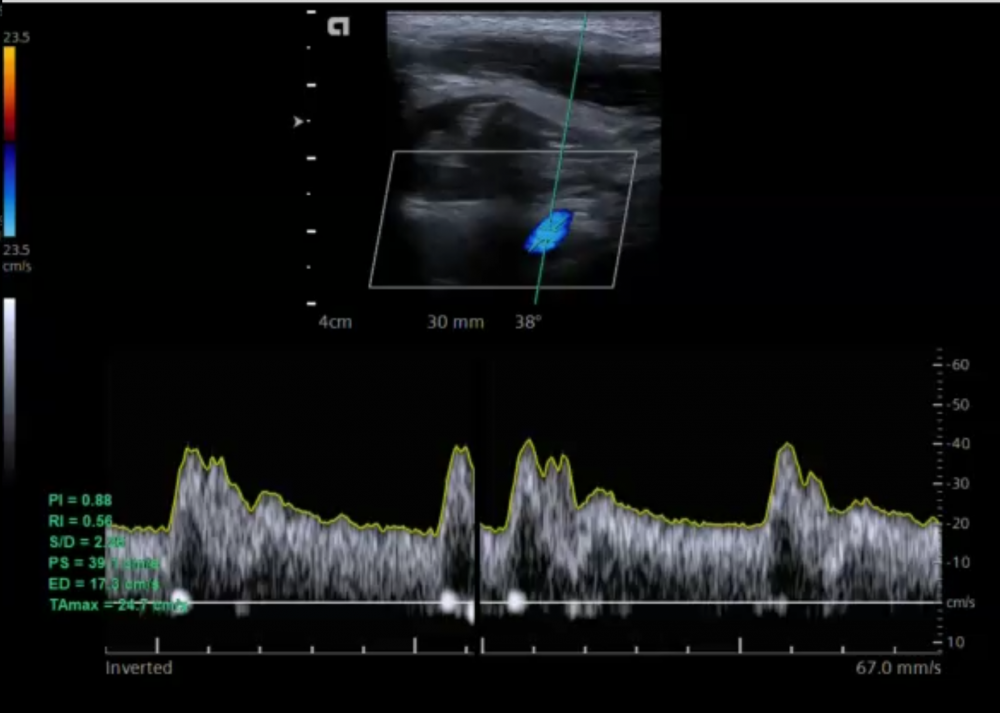 Va Spectral Doppler. Spectral Doppler of the vertebral artery. Typical pattern of a low resistance artery with rather high diastolic flow velocity relative to the systolic velocity (systolic / diastolic velocity ratio = 2.
Va Spectral Doppler. Spectral Doppler of the vertebral artery. Typical pattern of a low resistance artery with rather high diastolic flow velocity relative to the systolic velocity (systolic / diastolic velocity ratio = 2.
7.7 How can I determine the direction of flow in the vertebral artery?
In the setting of a subclavian steal syndrome (occlusion of the proximal subclavian artery you will find a reversal of flow in the vertebral artery). In other words the detection of a reversal in flow will allow you to diagnose /suspect an occlusion of the subclavian artery stenosis. There are several ways how ultrasound can be used to determine the direction of flow
How to determine the direction of flow in the vertebral artery Color bar Use the color bar and the vessel orientation / flow to determine the direction of flow (see below) Compare CCA Compare the flow direction (color) with that of the CCA (displayed on the same image). Both should show the same direction of flow Compare with vertebral veins Compare the flow direction (color) with that of the vertebral veins PW Doppler Use PW Doppler for the direction of flow
.pagination .pager .pager__item { font-size: 12px; } .pagination .pager .pager__item--current { padding: initial; } .pagination { margin: 0; margin: 0 auto; margin-top: 0 !important; } .pager { margin-top: 0 !important; padding: 0; display: flex; } .pagination .pager { padding: 0; } .pagination .pager a { padding: 8px 12px; } .pager__item a { box-shadow: none !important; } .aut-nav-carotid-p { text-align: center !important; margin-bottom: 6px !important; } function advagg_mod_2() { // Count how many times this function is called. advagg_mod_2.count = ++advagg_mod_2.count || 1; try { if (advagg_mod_2.count <= 40) { var autNaviCarotid1 = ('\ \
- \
- \
Chapters\
\
- \ 1\ \
- \ 2\ \
- \ 3\ \
- \ 4\ \
- \ 5\ \
- \ 6\ \
- \ 7\ \
- \ 8\ \
- \ 9\ \
- \ 10\ \
- \ 11\ \
- \ 12\ \
- \ 13\ \
- \ 14\ \
- \ 15\ \
- \ last »\ \ \ \ '); var autNaviCarotid2 = ('\
Carotid Ultrasound Webbook & Wiki\ \
- \
- \
‹ previous\
\
- \ BACK TO OVERVIEW\ \
- \ next ›\ \ \ \ '); (function($) { $(document).ready(function(){ $(".sonopl-article.sonopl-book__content.sonopl-content-main") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); $(".aut-nav-carotid") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); }); }(jQuery)); // Set this to 100 so that this function only runs once. advagg_mod_2.count = 100; } } catch(e) { if (advagg_mod_2.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_2, 250); } } } function advagg_mod_2_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_2(); } else { window.setTimeout(advagg_mod_2_check, 250); } } advagg_mod_2_check();
If you like the way we teach, please leave a message!
- \ BACK TO OVERVIEW\ \
- \ 1\ \


