Frozen Stream
Nature provides several opportunities to understand echocardiographic findings. Have you ever wondered what causes a river to freeze in the winter? It is the temperature of the water and the velocity of the flow of water in it.
To see how this relates to echo, read the following case:
Stanislaus, 43 years old, had received the diagnosis of cardiomyopathy several years ago. It was a big shock to him. However, he was doing fine at the time. His exercise capacity was limited, but he was active and even cycled on his home trainer.
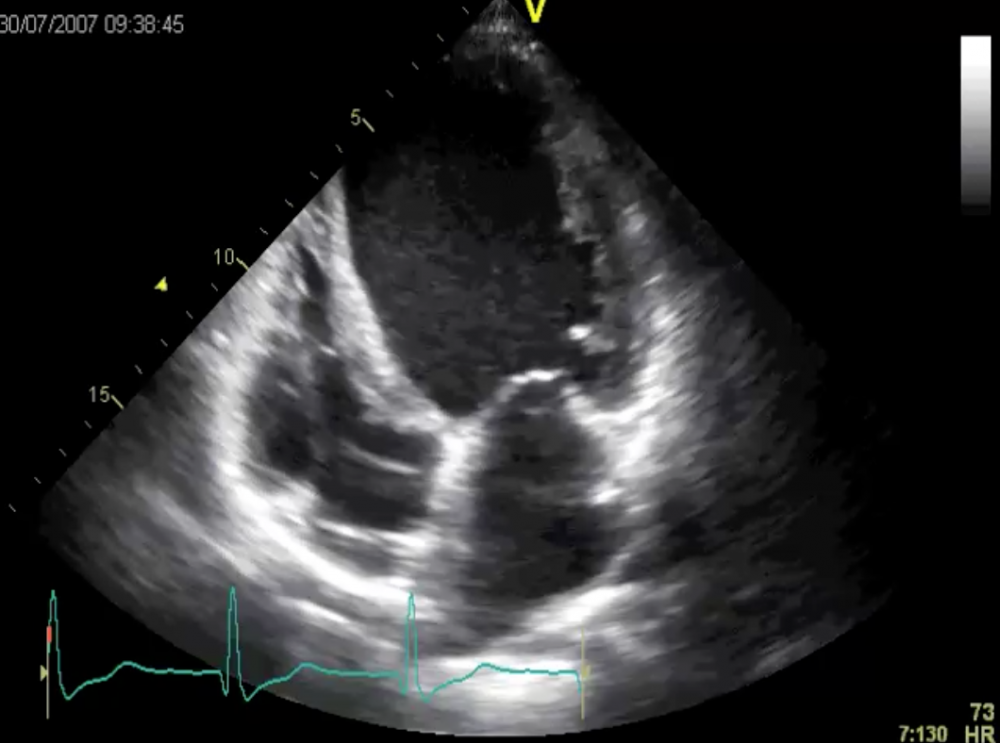 Four-chamber view: the ventricle is severely dilated and left ventricular function is poor.
Four-chamber view: the ventricle is severely dilated and left ventricular function is poor.
His left ventricle is dilated and its function is poor. However, note that his right ventricular function was still fine. This is usually a good sign and correlates with the patient’s symptoms. Also note the pacemaker leads in the right heart. Stanislaus had just received an ICD/CRT system. We hoped he would benefit from the device.
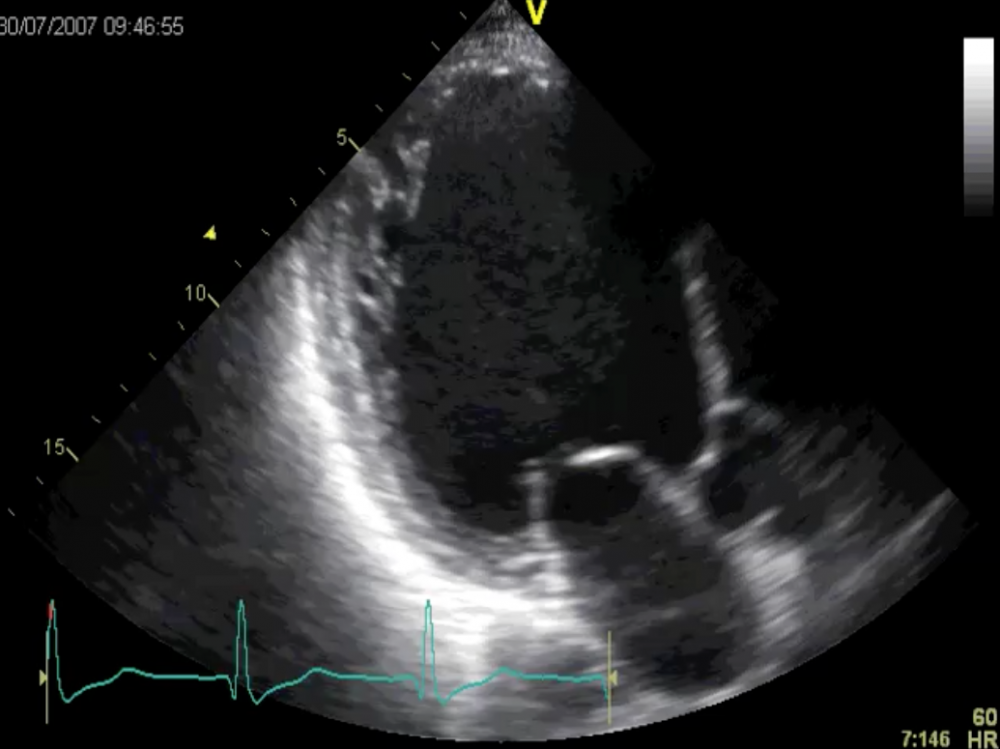 Apical long-axis view: global dysfunction.
Apical long-axis view: global dysfunction.
On a side note: look at the morphology of the posterolateral wall. Doesn’t the myocardium look rather spongy? Maybe he even has a “non-compaction” syndrome. However, this is not the point I’m trying to make.
Let us look at his echo just 3 years later:
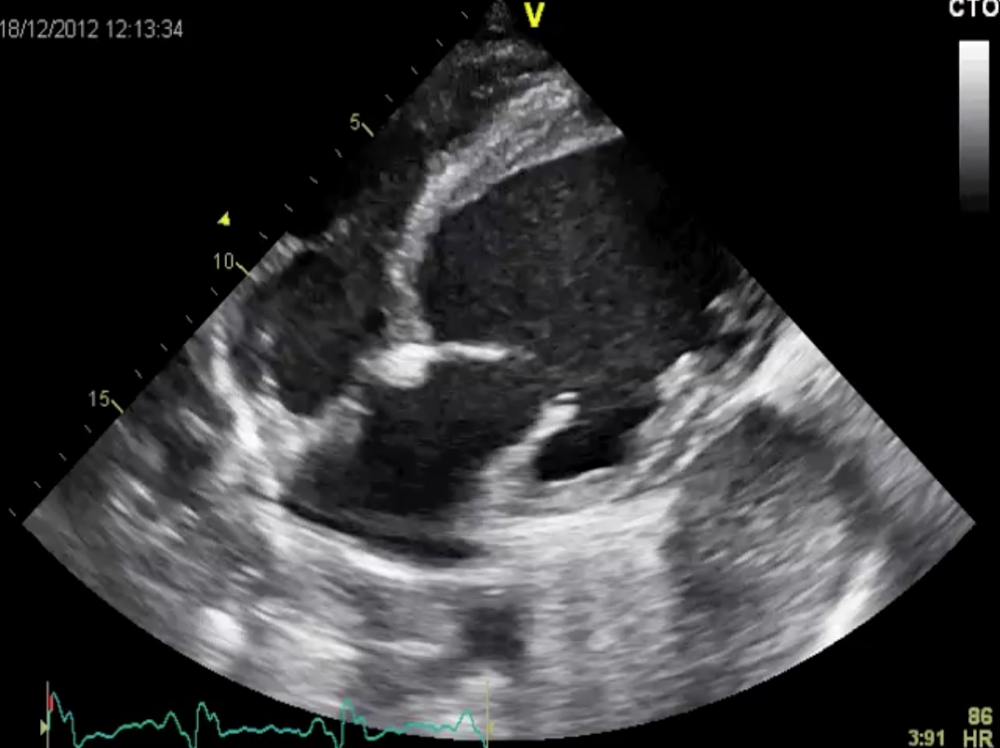
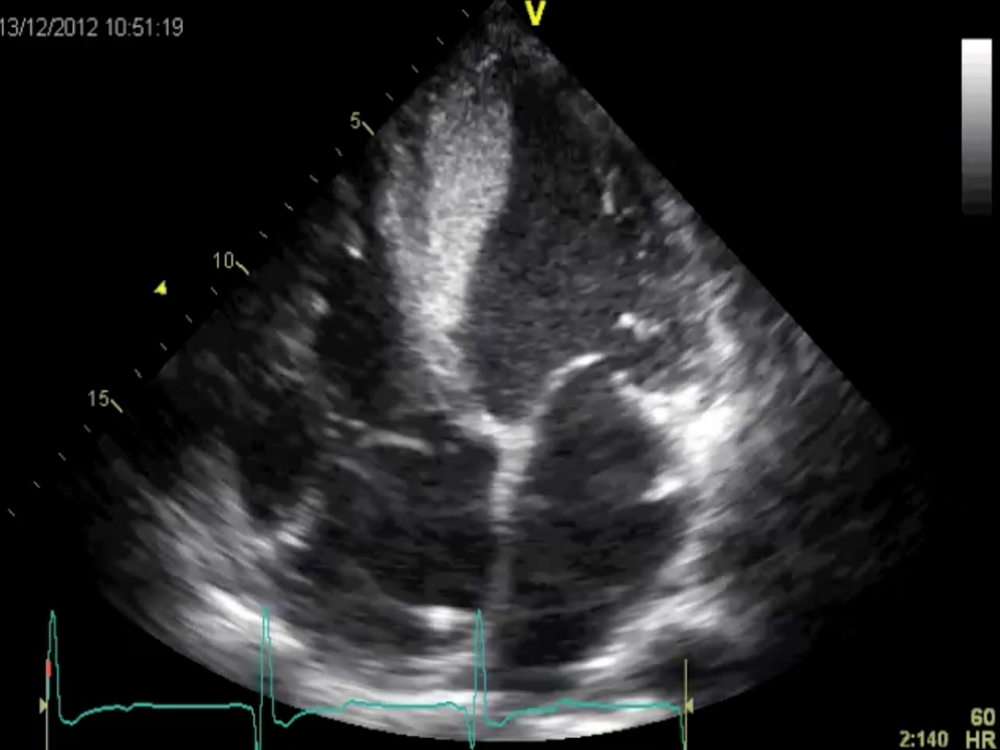 Four-chamber view of the left ventricle: the ventricle looks quite different now.
Four-chamber view of the left ventricle: the ventricle looks quite different now.
The ventricular wall (specifically the septum) is coated with a structure. If you look closely you can even see the flow of blood in the remaining cavity of the left ventricle. This is observed when left ventricular function is poor. Those who read our newsletters regularly will know of a similar case: “Chef de Jour”.
When we performed this echo, Stanislaus was truly symptomatic. His blood pressure was low, his limbs cold, and he had dyspnea at rest. Just for purposes of comparison, here is his apical long-axis view:
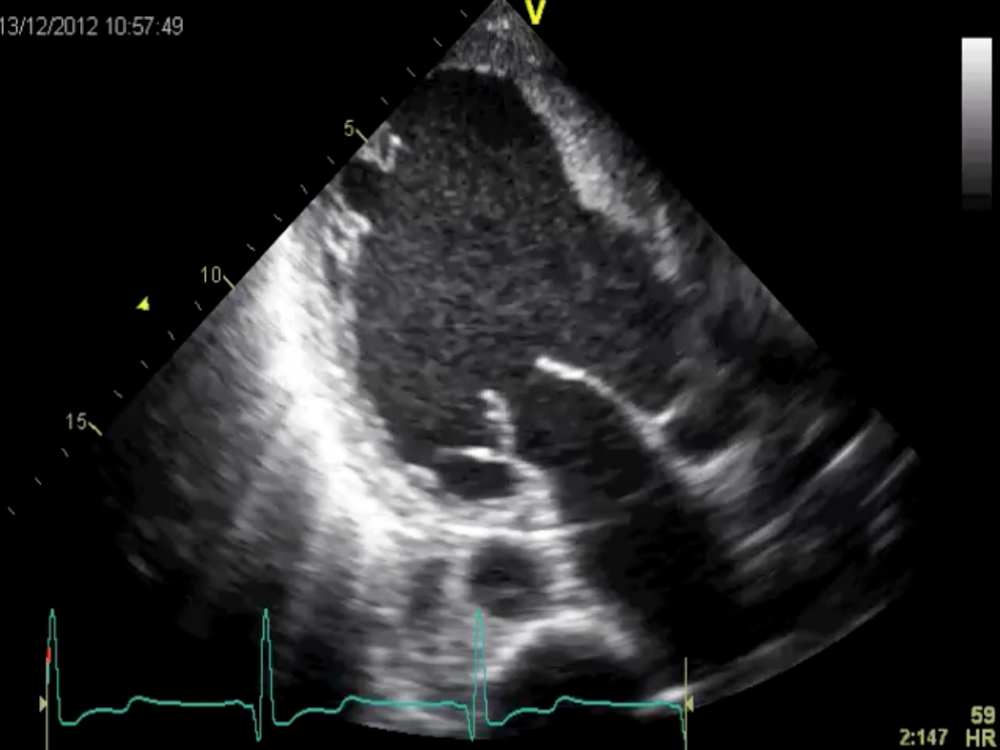 Apical long-axis view when he was in shock.
Apical long-axis view when he was in shock.
Compare this view with the previous apical long-axis view. His left ventricular function was poor at the time, but it is catastrophic now. Can you see how important it is to directly compare images "side by side"?
The extent of left ventricular dysfunction can also be appreciated on the subcostal view. Note that right ventricular function has also worsened now.
 Subcostal view: there is significant dyssynchrony despite CRT therapy. Both left and right ventricular function is reduced.
Subcostal view: there is significant dyssynchrony despite CRT therapy. Both left and right ventricular function is reduced.
In this setting, the coating on the left ventricle MUST be a thrombus. Slow flow of blood, as seen here, is a risk factor for thrombus formation. However, this is not the end of the story. Here is his cardiac CT:
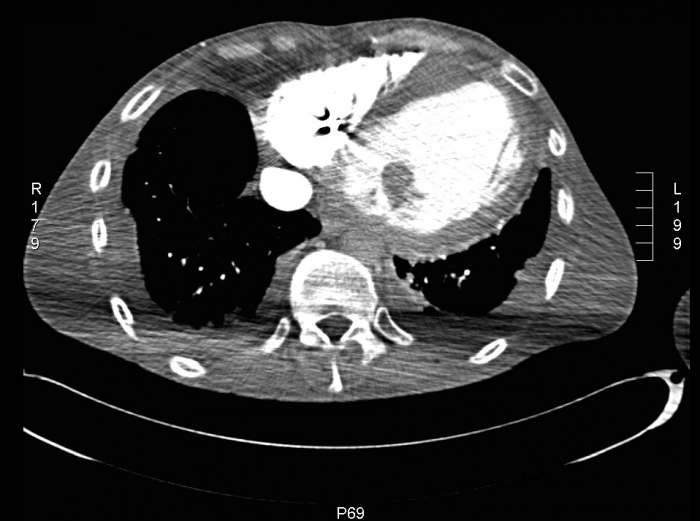 Cardiac CT: a thrombus is seen in the left ventricle.
Cardiac CT: a thrombus is seen in the left ventricle.
 CT scan: Obstruction of the iliac arteries at the bifurcation. Thrombus in the left ventricle and obstruction in the subclavian arteries as well.
CT scan: Obstruction of the iliac arteries at the bifurcation. Thrombus in the left ventricle and obstruction in the subclavian arteries as well.
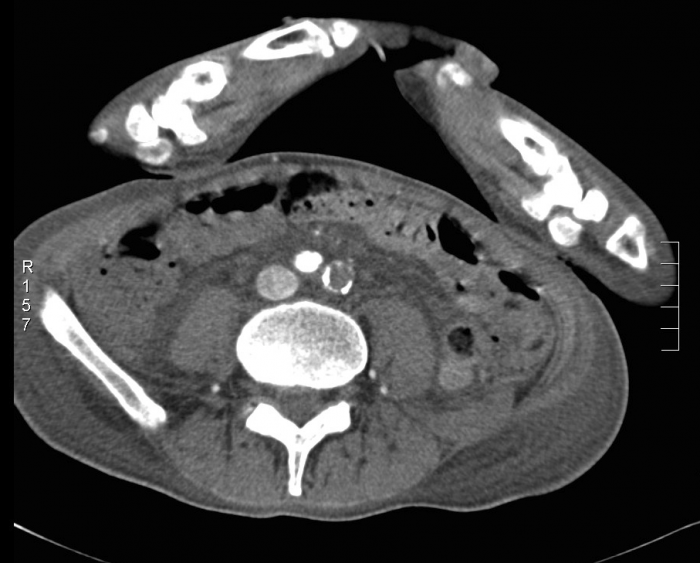 CT scan with thrombus in both iliac arteries.
CT scan with thrombus in both iliac arteries.
A very unique CT scan. Stanislaus has thrombotic obstruction of the subclavian arteries and a thrombus in the left ventricle. Now take a look at the aorta: there is no flow in the distal aspect of the aortic bifurcation. Thrombotic masses occlude the iliac arteries as well. This type of occlusion is named after a French surgeon who linked this pathology with the anatomy of the condition. It is known as the Leriche syndrome. These patients have claudication, no or weak femoral pulses, and suffer from impotence. Usually it is associated with atherosclerosis and other risk factors for vascular disease. Stanislaus did not have such risk factors. We assume that poor flow in the aorta due to low cardiac output and elevated peripheral vascular resistance was the cause of the Leriche syndrome.
Doesn’t this compare well with the frozen river? No matter how cold it is, as long as a river flows swiftly it rarely freezes. Stanislaus' blood flow may be compared with a river in which water flows too slowly.
How does the story end? Despite high-dose anticoagulation the thrombus could not be resolved as rapidly as we wished. The patient went into multiple organ failure and died shortly after we recorded the images you see here.
A sad ending again.
We hope to have something with a positive ending the next time, so watch your inbox. If you can’t wait to get more exciting teaching material from us, visit our blog (123sonography.com/blog). We have more than 100 entries with cases, tips and tricks, and interviews.
Yours,
Jamil & Thomas



