12.2 Anatomy and function of the mitral valve
12.2.1 The mitral valve leaflets
The mitral valve is a fairly complex structure. The name stems from the "mitra" or bishop's hat, which has two "tips" that resemble the two leaflets of the mitral valve, namely the anterior and the posterior leaflet.
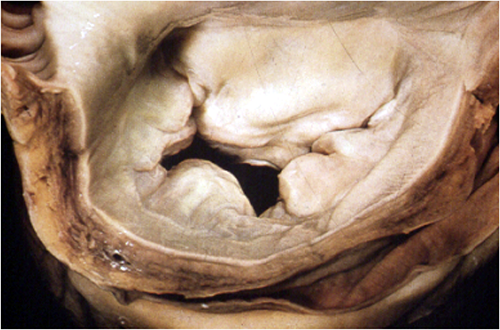
The anterior leaflet is longer and is positioned adjacent to the intervalvular fibrosa. Thus, it is in close proximity to the aortic valve (left and acoronary cusp). The posterior leaflet is shorter, but encompasses more (three fifths) of the annulus. Thus, actually both leaflets have approximately the same size with respect to their surface area. When looking at the posterior mitral valve from the left atrium, you will note small "bumps and indentations" which constitute the so-called scallops. In contrast, the anterior leaflet is much smoother; it has no indentations along its free edge.
We use Carpentier's classification to distinguish between the individual regions of the mitral valve. Both the anterior (A) and the posterior (P) leaflet are divided into three sections: anterolateral (1), middle (2), and posteromedial (3). Segment A1, for instance, would correspond to the anterolateral portion of the anterior leaflet while P2 would be the middle segment of the posterior leaflet, and so on. These segments do not always correlate with individual scallops, especially because the morphology of the valve may vary markedly. Some leaflets have three, while others four or even more "scallops". The segments in which the anterior and posterior leaflets "connect" are referred to as commíssures (anterolateral AL and posteromedial PM).
Study the anatomy of the mitral valve. Look at real specimens. Go to the operating room and see what a "real" mitral valve looks like.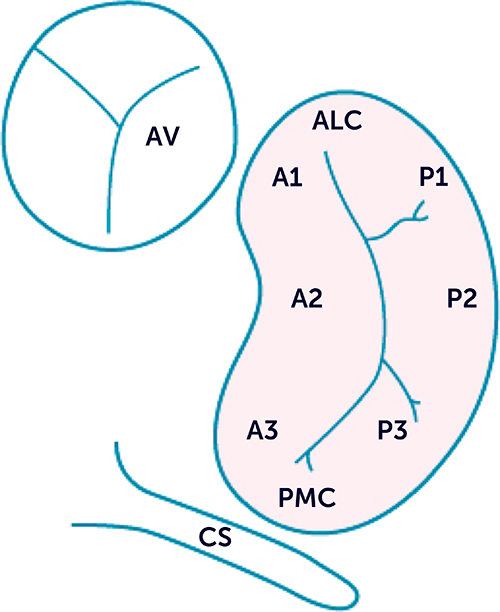
The line of coaptation is slightly bent (U-shaped) and the tips of the leaflets "curl" towards the ventricle. The leaflets touch each other not just at one point but along a surface, looking similar to "praying hands".
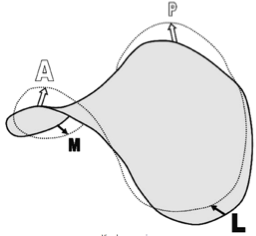
This region is referred to as the "coaptation zone" and its depth is known as "coaptation depth". The overlap of the leaflets is important for the competence of the valve. In a way it is a compensatory mechanism. When the mitral annulus dilates and the leaflets are dragged apart, there is still enough coaptation surface to maintain the function of the valve. Regurgitation occurs only when the annulus dilates further. The depth, area and length of this coaptation zone are important indicators of valve function and are used to make surgical or interventional (MitraClip) decisions. The triangular area defined by the leaflets and the plane of the annulus is known as the "tenting area". You will learn more about it when we discuss restrictive mitral regurgitation.
12.2.2 The orifice
The orifice of the mitral valve is more or less elliptical, resembling a bean.
Ranging in size between 4 and 6 cm2, it is a little smaller than the orifice of the tricuspid valve.
The plane of the valve is not flat but resembles a saddle. Recent investigations have shown that the saddle shape plays an important role in the distribution of forces that act on the mitral valve. The size of the annulus and the "high points" of the saddle vary considerably during the cardiac cycle. In normal individuals the area of the mitral valve is reduced by 10-15% during systole.
The geometry as well as the extent of dynamic changes are affected by cardiac disease. In dilated ventricles the annulus is more round and the motion of the annulus is reduced.
12.2.3 The subvalvular apparatus
The subvalvular apparatus consists of the papillary muscles and the chordae, which connect the mitral valve to the papillary muscle. One usually finds two papillary muscles: one arising from the apical and one from the middle third of the left ventricle. The anterolateral muscle has one "head" while the posteromedial muscle commonly has two heads. The papillary muscles also contract and shorten (by approximately 4 mm) during systole. This contributes to closure of the mitral valve. Due to the attachment of the papillary muscle to the walls of the ventricle, geometric abnormalities of the ventricle also affect the mitral valve and its function. In the section on functional mitral regurgitation you will see how this can affect the competence of the mitral valve.
The mitral valve is supported by three types of chordae, namely the marginal (primary), intermediate (secondary) and basal ones. The intermediate chordae are able to withstand strong forces while the primary chordae play an important role in relieving load during early stages of mitral valve closure.
12.2.4 Opening and closure of the valve
Closure of the mitral valve is a result of the complex interaction of several factors. The first factor is a rise of pressure in the left ventricle during contraction while the second factor is contraction of the papillary muscle which supports the valve. It has been speculated that vortex flow might act as an additional force in pressing the valve shut. Opening of the mitral valve during early diastole is a passive phenomenon caused by a rise in atrial pressure that exceeds the pressure in the left ventricle. In the early phase of filling, suction of the ventricle (recoil) also contributes to filling. Recent studies have shown that descent of the annulus plays a role. The ventricle "engulfs" a part of the volume of the left atrium. During diastasis the mitral valve is nearly closed (some backflow may occur in this phase). During atrial contraction the mitral valve is again pushed open.
In summary, the mitral valve and its entire apparatus is a complex structure, roughly resembling a parachute. Its function is closely linked to pressure differences between the atrium and the ventricle, as well as the left ventricle and its function.
