15. Carotid Endarterectomy and Stenting
/* .lity-iframe-container iframe { background: #fff !important; } */ .articles__categories nav { display: none !important; } .sonopl-book__aside .articles__categories { background: #f5f5f5; } .sonopl-article th, .sonopl-article td { color: black; text-align: left; } function advagg_mod_1() { // Count how many times this function is called. advagg_mod_1.count = ++advagg_mod_1.count || 1; try { if (advagg_mod_1.count <= 40) { var getClass = document.querySelectorAll(".articles__categories"); var a = document.createElement('a'); var linkText = document.createTextNode("Get Carotid MC Free Lectures"); a.appendChild(linkText); a.title = "newsletter"; a.href = "/overlay/forms/cu_mc/16618"; a.setAttribute("class", "sonopl-button sonopl-button--default"); a.setAttribute("data-lity", ""); a.style = "line-height: 1.2;margin-top: 25px;padding: 15px;width: 100%;"; for(var ix = 0; ix < getClass.length; ix++) { getClass[ix].appendChild(a) } // Set this to 100 so that this function only runs once. advagg_mod_1.count = 100; } } catch(e) { if (advagg_mod_1.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_1, 250); } } } function advagg_mod_1_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_1(); } else { window.setTimeout(advagg_mod_1_check, 250); } } advagg_mod_1_check();
15.1 What is carotid endarterectomy (CEA)
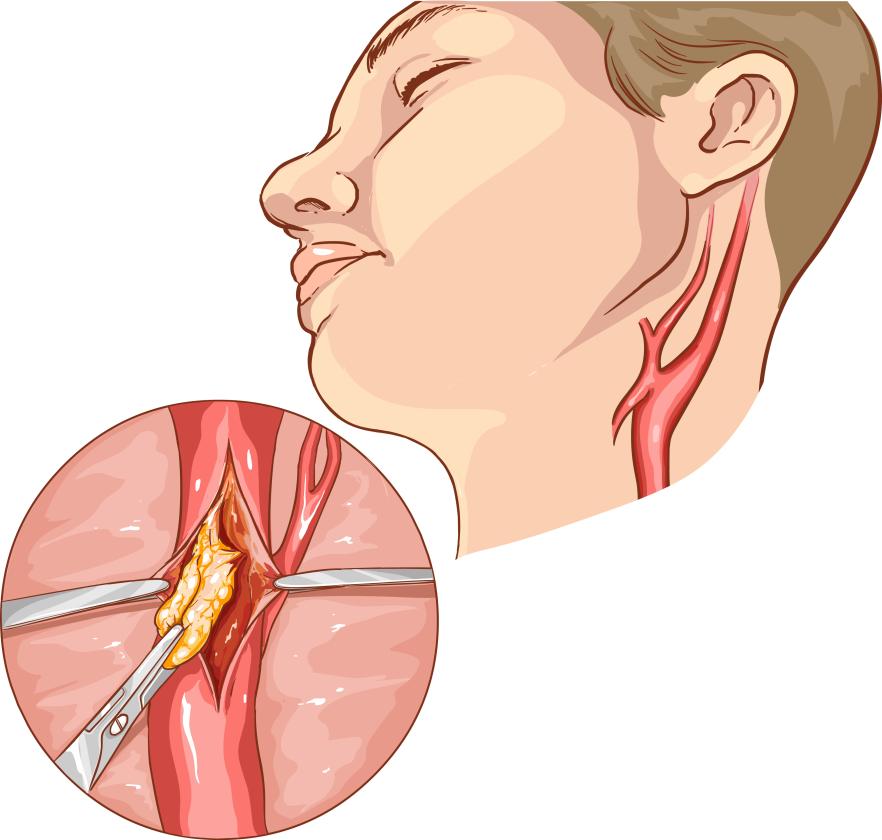
Carotid endaretectomy is a surgical procedure where the carotid artery is opened and the plaque is removed. The procedure allows restoration of blood flow and removal of embolic material to reduce the risk of ischemic / embolic stroke and TIA. There are two main techniques: the classical/conventional method where a patch is used to enlarge the vessel and the eversion method, where the carotid artery is transected at the bifurcation and then everted to remove the plaque. The artery is then repaired by performing an “end-to-end” anastomosis. The procedure is conducted either under local or general anesthesia.
 Carotid endarterectomy. The artery is cut open and the plaque is pealed off of the vessel
Carotid endarterectomy. The artery is cut open and the plaque is pealed off of the vessel
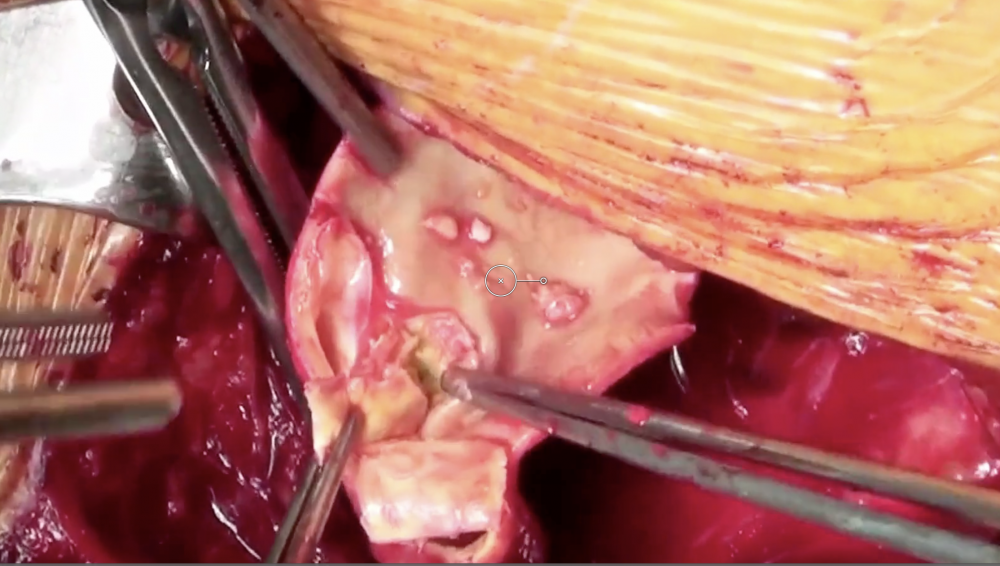 Surgery Video. Video demonstrating how the plaque is pealed off of the artery during carotid artery endarterectomy
Surgery Video. Video demonstrating how the plaque is pealed off of the artery during carotid artery endarterectomy
15.2 What are potential complications of carotid endarterectomy
- Stroke (embolic) and death
- Bleeding + haematoma
- Cranial nerve damage (facial nerve, hypoglossal nerve, vagal nerve, superior laryngeal nerve, glossopharyngeal nerve)
- Wound infection
- Hyperperfusion syndrome
- Restenosis
15.3 What is carotid artery stenting?
Carotid stenting is a percutaneous procedure where a stent is placed into the area of stenosis to expand the lumen and prevent vessel recoil. The procedure is performed under fluoroscopic guidance and an embolic protection device. Carotid artery stenting is an alternative to endarterectomy.
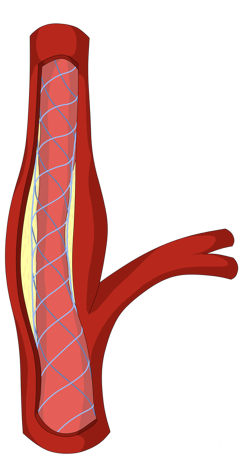 Stenting. Stenting of the Carotid artery. The stent is placed inside the vessel to expand the lumen.
Stenting. Stenting of the Carotid artery. The stent is placed inside the vessel to expand the lumen.
15.4 What are potential complications of carotid artery Stenting?
Risks include:
- Stroke and intracranial hemorrrhage and death
- hypoperfuison and bradycardia
- contrast complications
- carotid perforation
- carotid artery dissection.
- Bleeding + haematoma (site of vascular access)
- Acute stent thrombosis (very uncommon)
15.5 When is carotid endarterectomy indicated?
The indication for surgery is always a trade off between the benefit of the procedure and risk. Numerous large randomized studies such as the North American Symptomatic Carotid Endarterectomy Trial Collaborators (NASCET) and the European Carotid Surgery Trial (ECST) have clearly shown the carotid endarterectomy is beneficial in specific patient groups. The following table lists the current indications for this procedure.
- Patients with symptomatic severe (60-99%) stenosis are candidates for endarterectomy (CEA) or stenting if the procedural death / stroke risk is < 6%
- Symptomatic non-severe stenosis (>50%) if the procedural risk is < 6%
- Asymptomatic severe stenosis who are at high risk for stroke if the procedure risk is < 3% (stenosis progression, impaired cerebro- vascular reserve, spontaneous TCD embolisation)
- CEA is contraindicated in patients with < 50% stenosis
- CEA should be performed within 2 weeks of the patient’s last symptoms
- Carotid artery occlusion is NOT an indication for CEA - unless it is an acute occlusion
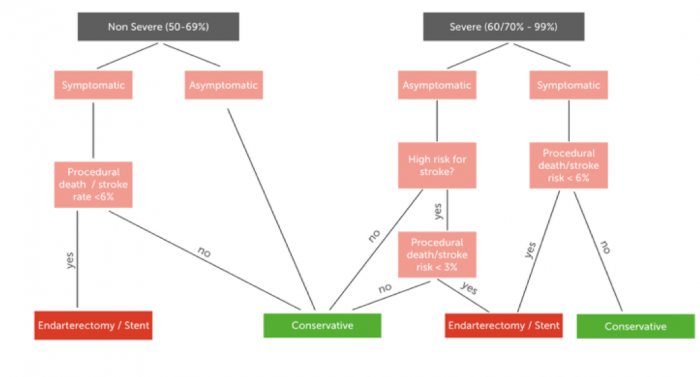 Flow chart depicting the indications for conservative therapy and carotid artery stenting/endarterectomy in patients with severe vs non-severe carotid artery stenosis
Flow chart depicting the indications for conservative therapy and carotid artery stenting/endarterectomy in patients with severe vs non-severe carotid artery stenosis
15.6 Which factors should be considered for carotid endarterectomy and stenting?
There are many other factors which must be considered when deciding if a percutaneous or surgical intervention should be performed.
Factors to be considered Neurologic symptoms TIA? Non-disabling stroke? Stroke? Note that isolated carotid stenosis does not cause vertigo, lightheadedness, or syncope Time since episode Ideally intervention should be performed within 4 days of an event. CEA is superior if early intervention is possible (within 3-4 weeks). Stenting is superior if late intervention is performed Degree of carotid artery stenosis 0-99% Location of stenosis Unilateral - bilateral (higher risk) Stenosis vs occlusion Collateral flow Co-morbitities Operative risk, survival? Vascular and local anatomic features Surgical challenges? Carotid plaque morphology High-risk plaque?
.pagination .pager .pager__item { font-size: 12px; } .pagination .pager .pager__item--current { padding: initial; } .pagination { margin: 0; margin: 0 auto; margin-top: 0 !important; } .pager { margin-top: 0 !important; padding: 0; display: flex; } .pagination .pager { padding: 0; } .pagination .pager a { padding: 8px 12px; } .pager__item a { box-shadow: none !important; } .aut-nav-carotid-p { text-align: center !important; margin-bottom: 6px !important; } function advagg_mod_2() { // Count how many times this function is called. advagg_mod_2.count = ++advagg_mod_2.count || 1; try { if (advagg_mod_2.count <= 40) { var autNaviCarotid1 = ('\ \
- \
- \
Chapters\
\
- \ 1\ \
- \ 2\ \
- \ 3\ \
- \ 4\ \
- \ 5\ \
- \ 6\ \
- \ 7\ \
- \ 8\ \
- \ 9\ \
- \ 10\ \
- \ 11\ \
- \ 12\ \
- \ 13\ \
- \ 14\ \
- \ 15\ \
- \ last »\ \ \ \ '); var autNaviCarotid2 = ('\
Carotid Ultrasound Webbook & Wiki\ \
- \
- \
‹ previous\
\
- \ BACK TO OVERVIEW\ \ \ \ '); (function($) { $(document).ready(function(){ $(".sonopl-article.sonopl-book__content.sonopl-content-main") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); $(".aut-nav-carotid") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); }); }(jQuery)); // Set this to 100 so that this function only runs once. advagg_mod_2.count = 100; } } catch(e) { if (advagg_mod_2.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_2, 250); } } } function advagg_mod_2_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_2(); } else { window.setTimeout(advagg_mod_2_check, 250); } } advagg_mod_2_check();
If you like the way we teach, please leave a message!
- \ BACK TO OVERVIEW\ \ \ \ '); (function($) { $(document).ready(function(){ $(".sonopl-article.sonopl-book__content.sonopl-content-main") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); $(".aut-nav-carotid") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); }); }(jQuery)); // Set this to 100 so that this function only runs once. advagg_mod_2.count = 100; } } catch(e) { if (advagg_mod_2.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_2, 250); } } } function advagg_mod_2_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_2(); } else { window.setTimeout(advagg_mod_2_check, 250); } } advagg_mod_2_check();
- \ 1\ \