How to assess cardiac filling and fluid responsiveness in neonates?
Scenario: You attended a term infant emergency cesarean section due to acute placental abruption and decreased fetal heart tone. After aggressive resuscitation including chest compression and resuscitation drugs, the infant responds and remains in poor condition – now being treated for ‘Hypoxic-ischemic encephalopathy (HIE) and acute respiratory failure.
First neonatal blood gas shows severe metabolic acidosis (pH<7) and sky-high lactate!
First rapid assessment: Infant has poor perfusion with delayed capillary refill (CRT 3-4 seconds), weak pulses, hypotension (mean blood pressure (BP) of 17-18mmHg) and looks pale.
Question: So, does this collapsed infant with severe hypoxic brain injury with hypotension and hemodynamic instability need fluid bolus, pressor, or careful wait-and-watch?
Traditional hemodynamic monitoring tools like blood pressure, heart rate, clinical examination, serum lactate, etc are NOT reliable in assessing cardiovascular well-being and assessing fluid status. They are proxy parameters and unreliable in estimating cardiac output, preload, afterload, cardiac contractility and assessing end organ perfusion. Giving unnecessary fluid bolus to neonate with cardiac failure or those with severely impaired cardiac function can lead to further deterioration.
Question: So, in emergent scenarios like this how could could you assess fluid status and determine whether infants needs fluid therapy or vasopressor medication?
Most clinicians would first give a fluid bolus ‘blindly’ assuming the infant will respond to fluid therapy. Cardiac point-of-care ultrasound (POCUS) can help in assessing fluid status, cardiac filling (pre-load), cardiac contractility and estimate cardiac output. Cardiac POCUS can help in understanding cardiovascular physiology and finding out what’s wrong and how to target a specific intervention.
Question: So, if you are are able to assess cardiac filling, contractility and cardiac function would you manage this infant differently?
Yes, if we know what is the underlying abnormal physiology then we can individualize the management and target specific intervention (precision medicine). Cardiac (POCUS) can be performed to assess the “feeling” (filling) and “emotion” (motion) of the heart. Direct ultrasound visualization can help to:
- Assess cardiac contractility and function by visual inspection
- Assess cardiac filling
- Inferior vena cava (IVC size) and collapsibility
- Variability in blood flow across LVOF (Velocity Time Interval, VTI)
Here are some practical tips to perform a neonatal cardiac POCUS in such a case of hypotension in a neonate:
Imaging Tips: Motion
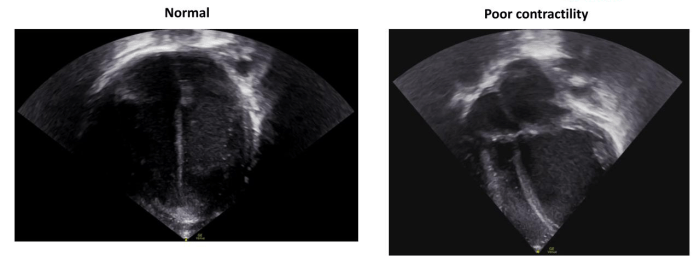
Cardiac contractility on visual inspection should be assessed using multiple views A4C, PLAX and PSAX. Here is an example of the A4C showing poor contractility and wall motion:
Imaging Tips: Filling
Cardiac filling on visual inspection should be assessed using multiple views apical 4 chamber (4AC), parasternal long (PLAX) and parasternal short (PSAX).
Here are the examples in 4AC:
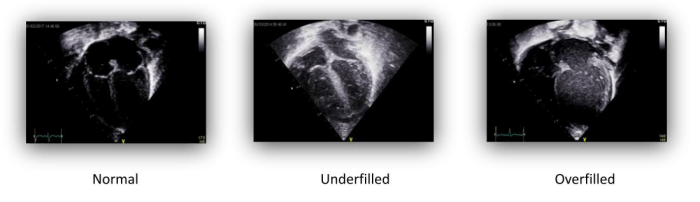
Caution on assessing cardiac output in children
Caveat: Newborn infant has physiological shunts including patent ductus arteriosus (PDA) and patent foramen ovale (PFO) which may contaminate assessing left and right ventricular output in neonates, especially during transitional circulation. These shunts direct blood flow differently than adult. The cardiac chambers size may be affected by the shunt size and the shunt flow direction.
Imaging Tips: IVC collapsibility
- Assessed in subcostal longitudinal view with marker towards head and probe tilting towards right
- IVC variability during inspiration and expiration
- IVC collapsibility index calculated by measuring IVC Dmax and Dmin diameters
- Collapsibility of >55% is predictive of fluid responsiveness
- IVC no-variability or dilated IVC because of hypervolemia, increased right atrial or increased intrathoracic pressure
- Caveat: IVC collapsibility index on infant on mechanical ventilation with positive thoracic pressure. IVC distensibility can be used in this situation instead.
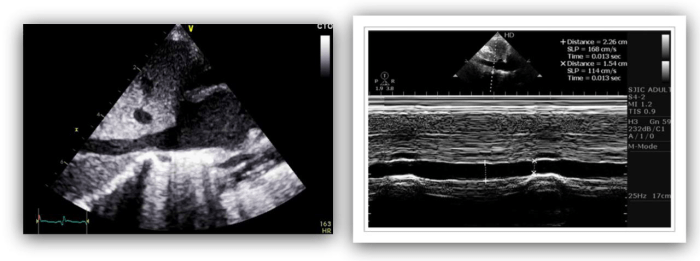 Normal IVC variability during inspiration and expiration
Normal IVC variability during inspiration and expiration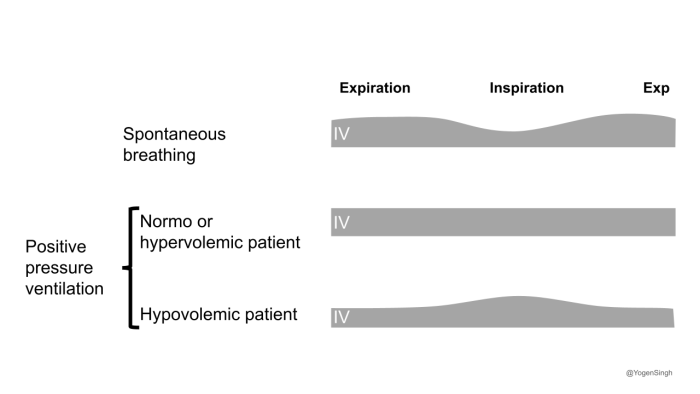
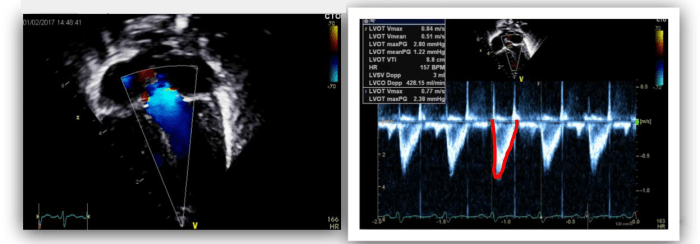
Imaging Tips: LVOT blood flow (VTI)
- LVOT blood flow measured in apical 5 chamber view. Obtain apical 5 chamber view by tilting the probe anteriorly (upwards) from 4AC
- Pulse wave doppler gated below the aortic valve to measure flow velocity, and Trace ejection wave, and record VTI
- >15% variability in blood flow (VTI) across LVOT suggest hypovolaemia and fluid responsiveness.
Other more complex echo measurements have been used to assess cardiac function and fluid responsiveness. The scanning tricks above are a good start for rapidly assessing cardiac filling (fluid status) and fluid responsiveness while managing critically ill neonates and children. performing serial assessment. These techniques can be used using to see response to intervention by assessing them on serial cardiac POCUS assessment.
If you have any other questions or want to learn more about how to perform perform cardiac POCUS or point of care echocardiography for different indications in neonates and children, please send me a message. I am looking to share more of my personal tips and tricks.
Best wishes,
Yogen



