Gemini Part I
As doctors we are usually responsible for the life of ONE patient. However, this is not always the case. We have to make rather complex decisions in some situations - when more than one life is at stake. The following is an example of this nature.
Good news at first
Brigitte, owner of a cosmetic parlor, was 40 years old when she first became pregnant. The pregnancy was not planned, but she was excited and looked forward to being a mother. Her next surprise was when discovered that she was carrying (monochorionic diamniotic) twins.
One of the two fetal hearts at 28 weeks.
Brigitte was told that she and her offspring were at risk - not only because of her diabetes but also because she was 40 and was carrying twins. Controlling her glucose levels with insulin was not a problem. Her blood pressure was fine and she felt well, at least until the 28th week of gestation. After this time she experienced shortness of breath for a few days, but was initially not worried about it. After all, her belly was already rather big. She thought it was merely the high diaphragm that caused dyspnea. However, her shortness of breath worsened rapidly and her legs started to swell. Her heart rate increased, and so did her blood pressure. Noting blood pressure levels of 190/110 mmHg, she finally consulted her gynecologist, who immediately admitted her to our hospital with signs and symptoms of heart failure.
A case for the cardiologist
I am sure most of you now believe that she has peripartal cardiomyopathy - similar to the case we presented several months ago (Link https://www.123sonography.com/blog/dyspnea-delivered-stork). However, the following image loop will show you that her left ventricular function was okay:
Four-chamber view showing normal left ventricular function.
Her ejection fraction was 69%. But there is something else: the ventricle is somewhat enlarged. Her end-diastolic volume was 123 ml. Now you might suggest that this may be due to the increase in blood volume during pregnancy. True, it does play a role but there is another potential cause. Here is the color Doppler study:
Color Doppler showing severe mitral regurgitation.
This is fairly severe mitral regurgitation and is contributing to left ventricular enlargement (left ventricular volume overload) and must be one of the causes of her symptoms. If you take a look at the velocity of the tricuspid signal, you will note that she has severe pulmonary hypertension.

TR signal. The maximum velocity is 4.2 m/sec.
Using the Bernoulli equation and adding an estimated 5 mmHg for right atrial pressure yields a systolic pulmonary artery pressure of more than 70mmHg. No wonder it was difficult to examine her in a supine position.
Trying to solve the mystery
What is the cause of mitral regurgitation in this case? Go back to the four-chamber view. The morphology of the mitral valve is completely normal and the direction of the jet is central. It looks as if she has a “functional” cause of mitral regurgitation. Probably annular dilatation. But why? She has normal global and regional left ventricular function.
I really don't know the answer. Did the initial increase in volume cause some leakage of the mitral valve, which then led to further dilatation and increased mitral regurgitation? In other words, did it lead to a vicious cycle that culminated in severe mitral regurgitation? She was diagnosed with preeclampsia, mild proteinuria, blood pressure values of about 150/90 mmHg, and slightly elevated creatinine levels (1.1 mg/dl). Her sodium levels were low: 124 mmol/l. Patients with preeclampsia are known to have altered hemodynamics, higher stroke volumes, ejection fractions, and higher systemic vascular resistance. We also know that patients with preeclampsia are subject to a high risk of cardiovascular disease. However, Brigitte had no symptoms of ischemia. Her ECG was normal, as were her troponin levels. Let us look at her longitudinal strain.
A second look at LVF
Longitudinal strain is a new way at looking at left ventricular function. We now know that it can be used as an early marker of left ventricular dysfunction.
Longitudinal strain: global longitudinal strain is normal but the pattern
is conspicuous.
She has a global peak systolic strain level of 19.3 %, which is normal. However, the pattern is unusual. The apical segments (center) are hyperdynamic (bright red) while longitudinal function is reduced (pink) in the basal segments (outer circle). Now all this is still speculative, but it seems as if the apical segments are compensating for reduced longitudinal contractility at the base. Despite her normal ejection fraction, myocardial function is not entirely normal. Poor longitudinal function has been frequently reported in patients with preeclampsia. However, I have not encountered a single case of mitral regurgitation induced by preeclampsia.
We need your help
What would you do in this setting? Pre-terminate the pregnancy? She is in the 28th week, so the twins do have a chance of survival. Wouldn’t it be better to postpone a cesarean section as long as possible? The treatment of choice is diuretics, but diuretics are not devoid of risks in pregnancy. They may lead to oligohydramnion and put the twins at risk. It is a difficult decision. I would be curious to know your suggestions. Please post them in the Facebook section below. I saw the patient recently. The decision has not been made yet, but I will give you a follow-up in one of the next newsletters.
Let's hope we can save three lives at once.
Thomas
-->
As doctors we are usually responsible for the life of ONE patient. However, this is not always the case. We have to make rather complex decisions in some situations - when more than one life is at stake. The following is an example of this nature.
Good news at first
Brigitte, owner of a cosmetic parlor, was 40 years old when she first became pregnant. The pregnancy was not planned, but she was excited and looked forward to being a mother. Her next surprise was when discovered that she was carrying (monochorionic diamniotic) twins.
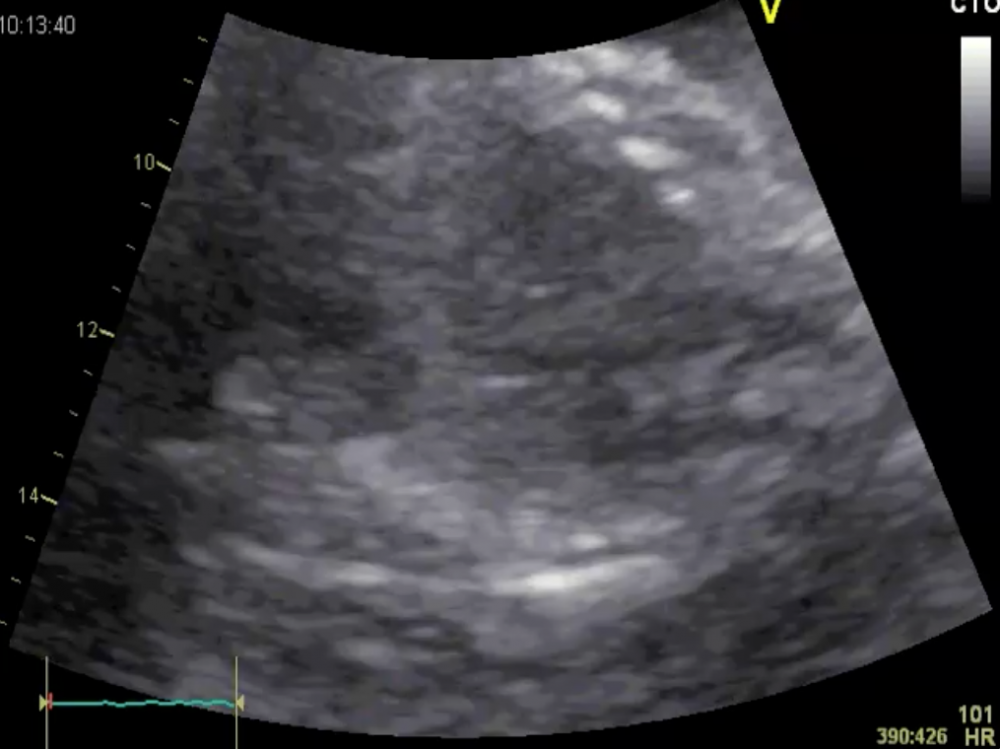 One of the two fetal hearts at 28 weeks
One of the two fetal hearts at 28 weeks
Brigitte was told that she and her offspring were at risk - not only because of her diabetes but also because she was 40 and was carrying twins. Controlling her glucose levels with insulin was not a problem. Her blood pressure was fine and she felt well, at least until the 28th week of gestation. After this time she experienced shortness of breath for a few days, but was initially not worried about it. After all, her belly was already rather big. She thought it was merely the high diaphragm that caused dyspnea. However, her shortness of breath worsened rapidly and her legs started to swell. Her heart rate increased, and so did her blood pressure. Noting blood pressure levels of 190/110 mmHg, she finally consulted her gynecologist, who immediately admitted her to our hospital with signs and symptoms of heart failure.
A case for the cardiologist
I am sure most of you now believe that she has peripartal cardiomyopathy. However, the following image loop will show you that her left ventricular function was okay:
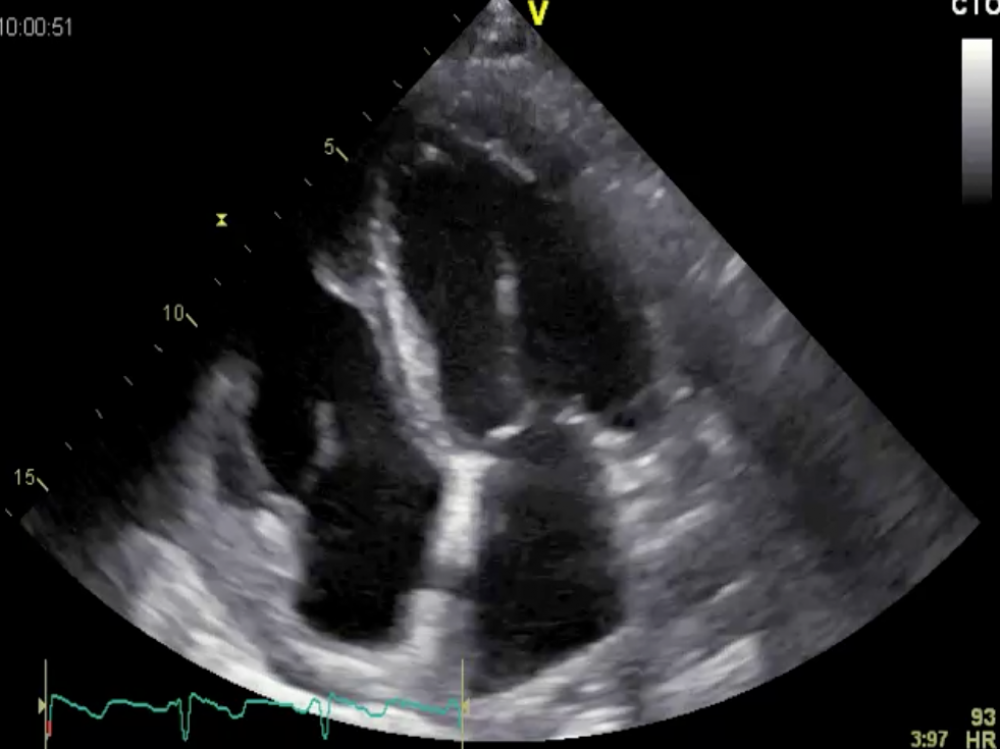 Four-chamber view showing normal left ventricular function
Four-chamber view showing normal left ventricular function
Her ejection fraction was 69%. But there is something else: the ventricle is somewhat enlarged. Her end-diastolic volume was 123 ml. Now you might suggest that this may be due to the increase in blood volume during pregnancy. True, it does play a role but there is another potential cause. Here is the color Doppler study:
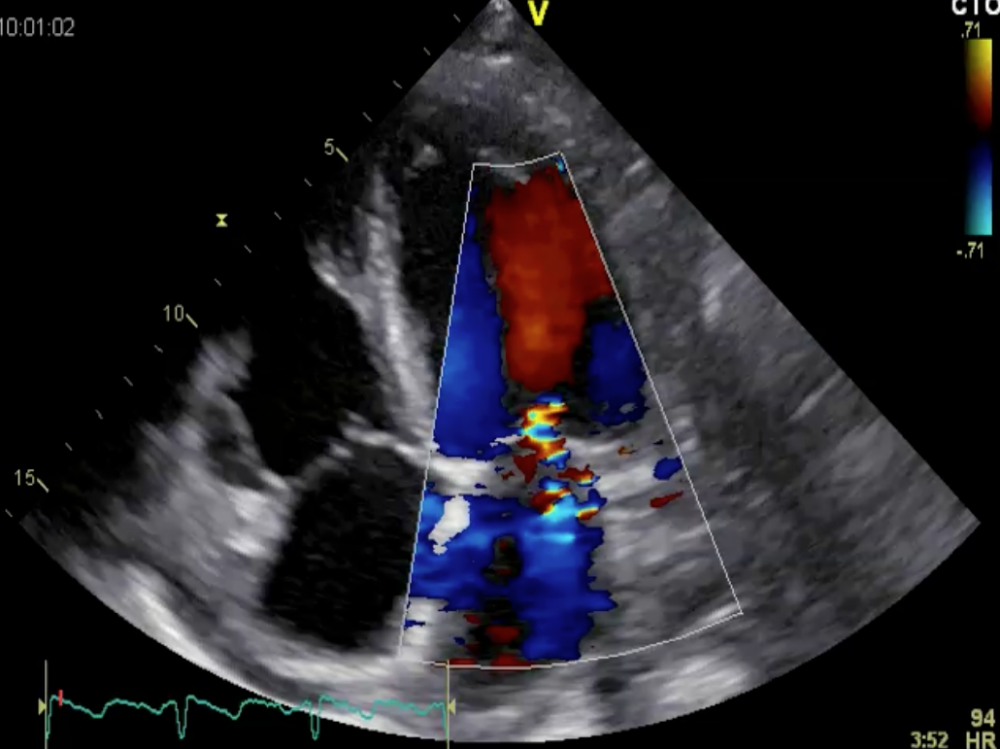 Color Doppler showing severe mitral regurgitation
Color Doppler showing severe mitral regurgitation
This is fairly severe mitral regurgitation and is contributing to left ventricular enlargement (left ventricular volume overload) and must be one of the causes of her symptoms. If you take a look at the velocity of the tricuspid signal, you will note that she has severe pulmonary hypertension.
 TR signal. The maximum velocity is 4.2 m/sec.
TR signal. The maximum velocity is 4.2 m/sec.
Using the Bernoulli equation and adding an estimated 5 mmHg for right atrial pressure yields a systolic pulmonary artery pressure of more than 70mmHg. No wonder it was difficult to examine her in a supine position.
Trying to solve the mystery
What is the cause of mitral regurgitation in this case? Go back to the four-chamber view. The morphology of the mitral valve is completely normal and the direction of the jet is central. It looks as if she has a “functional” cause of mitral regurgitation. Probably annular dilatation. But why? She has normal global and regional left ventricular function.
I really don't know the answer. Did the initial increase in volume cause some leakage of the mitral valve, which then led to further dilatation and increased mitral regurgitation? In other words, did it lead to a vicious cycle that culminated in severe mitral regurgitation? She was diagnosed with preeclampsia, mild proteinuria, blood pressure values of about 150/90 mmHg, and slightly elevated creatinine levels (1.1 mg/dl). Her sodium levels were low: 124 mmol/l. Patients with preeclampsia are known to have altered hemodynamics, higher stroke volumes, ejection fractions, and higher systemic vascular resistance. We also know that patients with preeclampsia are subject to a high risk of cardiovascular disease. However, Brigitte had no symptoms of ischemia. Her ECG was normal, as were her troponin levels. Let us look at her longitudinal strain.
A second look at LVF
Longitudinal strain is a new way at looking at left ventricular function. We now know that it can be used as an early marker of left ventricular dysfunction.
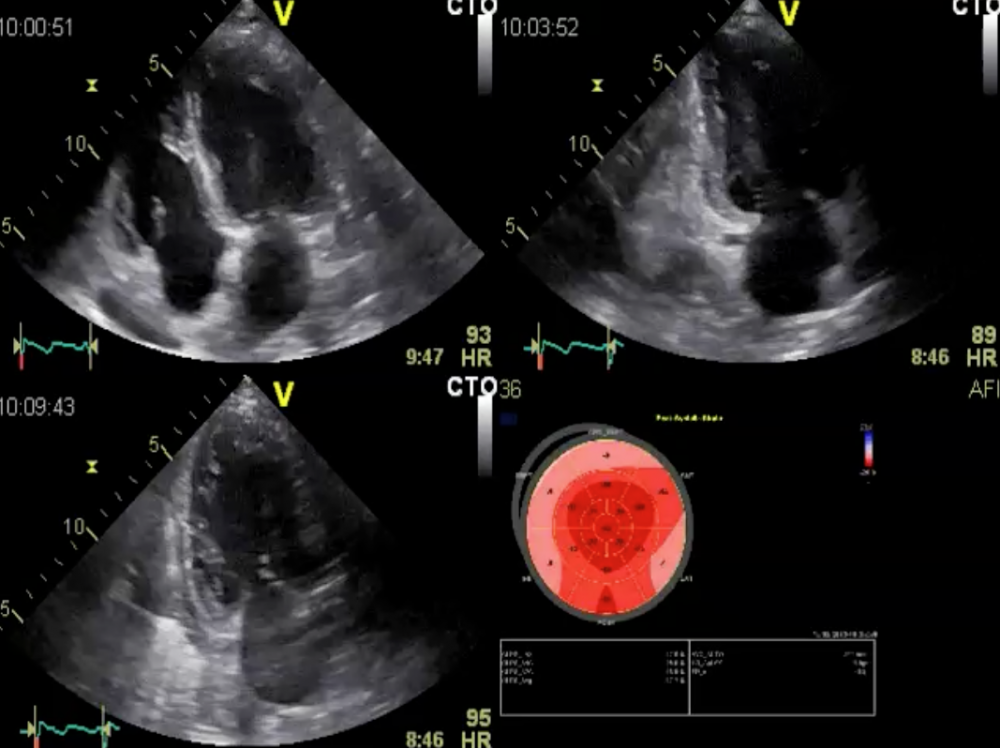 Longitudinal strain: global longitudinal strain is normal but the pattern is conspicuous.
Longitudinal strain: global longitudinal strain is normal but the pattern is conspicuous.
She has a global peak systolic strain level of 19.3 %, which is normal. However, the pattern is unusual. The apical segments (center) are hyperdynamic (bright red) while longitudinal function is reduced (pink) in the basal segments (outer circle). Now all this is still speculative, but it seems as if the apical segments are compensating for reduced longitudinal contractility at the base. Despite her normal ejection fraction, myocardial function is not entirely normal. Poor longitudinal function has been frequently reported in patients with preeclampsia. However, I have not encountered a single case of mitral regurgitation induced by preeclampsia.
We need your help
What would you do in this setting? Pre-terminate the pregnancy? She is in the 28th week, so the twins do have a chance of survival. Wouldn’t it be better to postpone a cesarean section as long as possible? The treatment of choice is diuretics, but diuretics are not devoid of risks in pregnancy. They may lead to oligohydramnion and put the twins at risk. It is a difficult decision. I would be curious to know your suggestions. Please post them in the Facebook section below. I saw the patient recently. The decision has not been made yet, but I will give you a follow-up in one of the next newsletters.
Let's hope we can save three lives at once.
Thomas