Detecting a Mistake
All humans make mistakes, including the best trained jet pilot, the professional mountain climber, or the skilled acrobat. The same is true of doctors. Fortunately, not all errors have catastrophic consequences. Quite often we are able to detect what went wrong before something goes seriously wrong. The following case illustrates how valuable echocardiography can be in detecting things that should have not happened.
Electric threat
Patrick is a survivor of sudden death, with a rather rare genetic condition known as the Brugada syndrome - an electrical abnormality that puts him at risk for lethal ventricular arrhythmia.
 Here is his ECG: note the typical ST elevations in the right precordial leads.
Here is his ECG: note the typical ST elevations in the right precordial leads.
The Brugada syndrome is marked by a right bundle branch block-like pattern and ST segment elevation in leads V1 to V3, which are wither cove or saddle back in shape.
Safety net
Obviously, the next step was to implant an ICD. However, this did not resolve Patrick's problem. After the implantation he suffered from recurrent supraventricular tachycardia, which was why he was brought to our hospital. Here is his transthoracic echo:
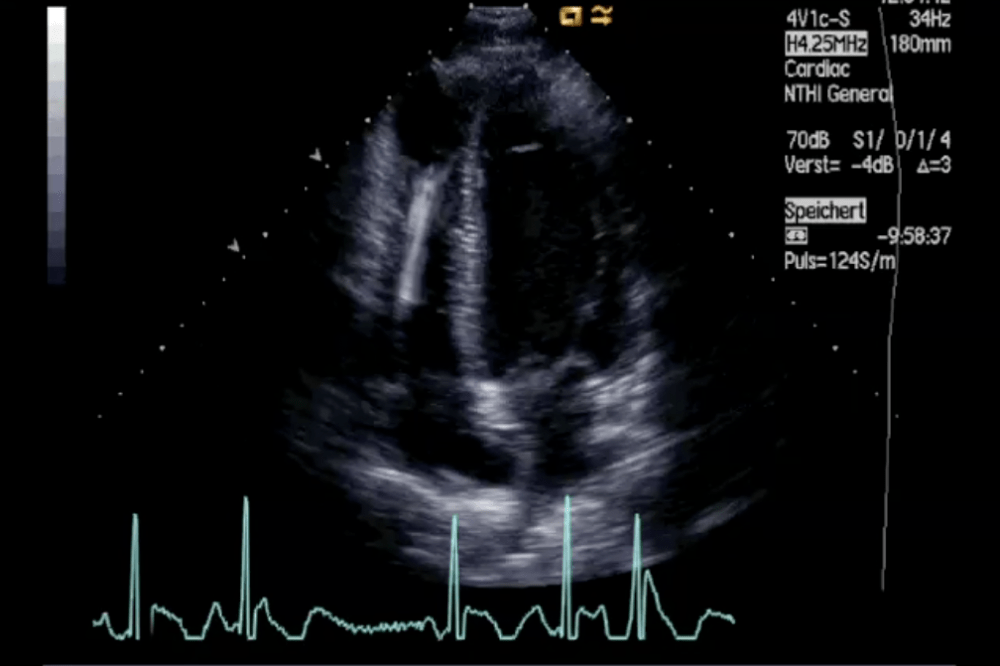 Normal four-chamber view with ICD leads in the right heart.
Normal four-chamber view with ICD leads in the right heart.
We didn’t find anything special on the transthoracic echo. His left ventricular function was normal and he had no pericardial effusion. The leads, we thought, were in correct position.
A problem..
He was scheduled for ablation therapy of his SVTs. A routine TEE study was performed before the procedure to rule out a thrombus.The left atrium, including the left atrial appendage, was free of thrombi. However, take a look at the ICD leads.
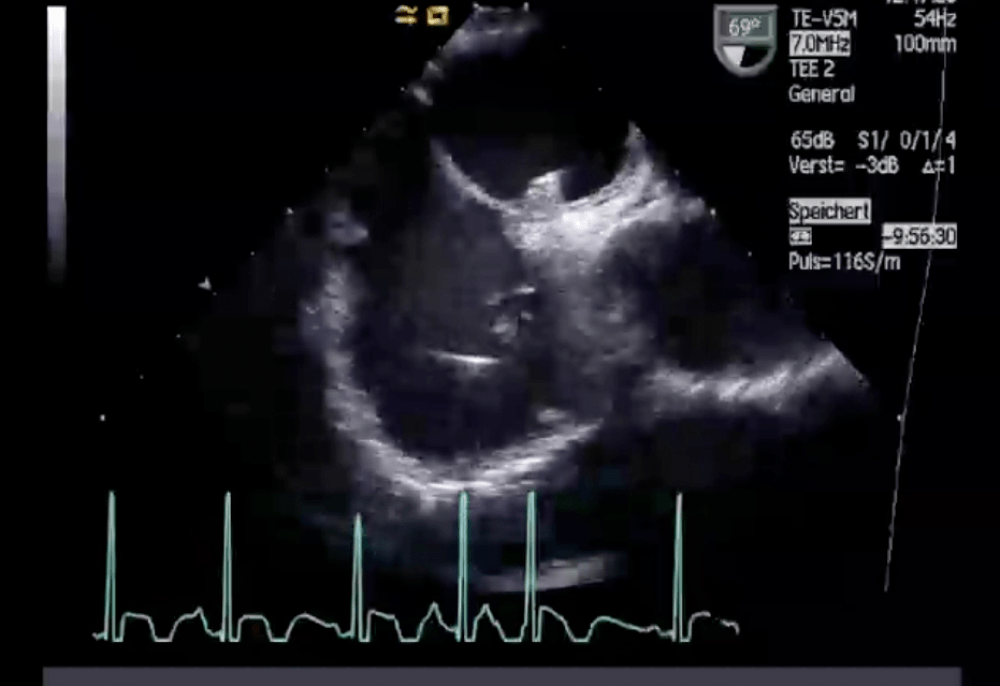 Bicaval view (TEE Study) showing the ICD leads. Note that something is dangling on the leads. The patient also had a bout of SVT during the recording of the loop.
Bicaval view (TEE Study) showing the ICD leads. Note that something is dangling on the leads. The patient also had a bout of SVT during the recording of the loop.
Can you see the structures on the leads? Certainly these are highly suspicious of thrombi or even vegetations. You can see them here in 3D in the following loop:
 Several structures are seen on the leads.
Several structures are seen on the leads.
Another problem
One more thing is pretty unusual. Can you see what his other problem is? Take a close look at the position of the lead.
 Bicaval view showing the atrial lead passing through a patent foramen ovale.
Bicaval view showing the atrial lead passing through a patent foramen ovale.
The atrial lead is incorrectly positioned. It passes through a patent foramen ovale - a rather unusual finding.
 3D study of the interatrial septum from the left atrium. You can see the lead poking through.
3D study of the interatrial septum from the left atrium. You can see the lead poking through.
Does this explain his supraventricular tachycardia? Maybe the abnormal lead position triggers the arrhythmia? How high is the risk of paradox emboli in this setting? How does one correct the problem? Does it matter at all? Should we just go on with the ablation or should we pull out the atrial lead, reposition it, and see whether that solves the SVT problem? What if the thrombi dislodge during the procedure?
Playing it safe
Eventually, we opted for the safest approach: surgical removal of the entire ICD system and closure of the PFO, followed by antibiotic treatment and re-implantation of a new ICD device. All went well. No further complications occurred. The pacemaker leads functioned well. However, Patrick still had recurrent supraventricular tachycardia. Thus, the incorrectly positioned lead was not the cause of his additional arrhythmia. It must have been associated with the Brugada syndrome (25-30% of patients with Brugada syndrome also have SVT). Successful ablation therapy was performed 3 months later. Now everything is fine.
 Four-chamber view showing that his condition had resolved.
Four-chamber view showing that his condition had resolved.
Sure, one could have suspected the abnormal position of the lead from the chest X-ray, but in this case echo was definitely the hero!
Echo assistance
An unusual case indeed, but it shows you that you must be aware of potential complications that may occur after pacemaker and ICD implantation. Most of all, echo is an important tool for interventionalists and surgeons in finding things that go wrong sometimes.
Best,
Thomas
PS: If you are interested in other echo cases that deal with pacemakers here is another entry called “Wiggles” that you should read.
PPS: Do you have similar echo’s dealing with iatrogenic problems? Why not share them with us? We all want to learn from mistakes.


