Category
Tips & Tricks
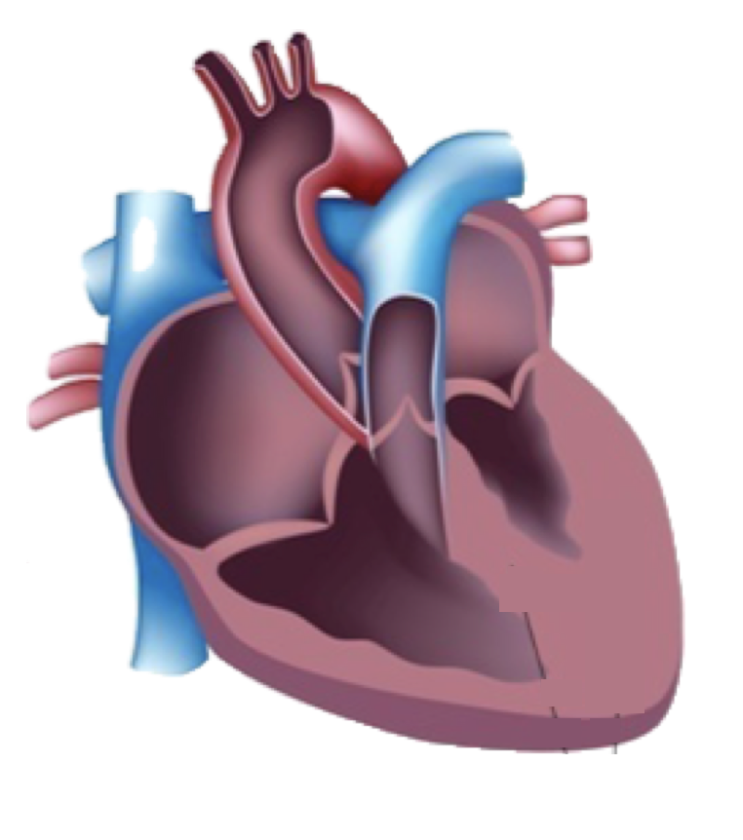
Common mistakes - Left Ventricular Hypertrophy
1) Don´t use MMode to assess LVH
That’s what I did when I started with echocardiography. Off course back then this is what the guidelines recommended. But in the meantime we know that the M-Mode line rarely cuts the ventricle perpendicular. This means you will often overestimate the thickness of the myocardium. 2D Echo is what you should use.My Tip: Perform several 2D measurements both from a parasternal (long and short) and apical view (angulated 4-chamber view)
2) The moderator band is included into the measurement
Both the moderator band and RV trabecula can lie adjacent to the interventricular septum. Sometimes it is difficult to delineate them from the septum. But including them into your measurement can lead to significant overestimation of septal thickness.My Tip: angulate the transducer until you get a view where you can clearly delineate the moderator band from the septum. Use this view for your measurement.
2) Measuring the thickest part of the septum
We all know the thickness of the septum varies and quite frequently you will see a buldge in the proximal portion. Measuring septal thickness there is not representative of the entire ventricleMy Tip: : Describe the shape of the septum and provide detailed information on where you measure. Summarize you impression (hypertrophy yes or no and how severe) based on all measurements. Alternatively you can also calculate the LV mass.
3) The findings are not put into a clinical context
A millimeter up or down can make a huge difference for the patient. Is he healthy or not? Is hypertrophy present? And you don’t want to make someone sick just based on the tiny motion of the trackball when you perform the measurement. While we have cut off values, be aware that the thickeness of the septum will be different in someone who has a body surface area of over 2.3m2, opposed to someone who is small. Clearly it is also important to know if someone has hypertension or not.My Tip: Talk to the patient, find out more about him. Is he hypertensive? Does he do lots of sports?
4) Not actively looking for apical hypertrophy
Apical hypertrophic cardiomyopathy can easily be missed, especially when you are foreshortening the left ventricle, your gain settings are set low or the image quality is poor. Sure you can use contrast, but first you have to have the suspicion.My Tip: Make sure you always see the endocardial and epicardial boarder of the myocardium at the apex. Only then will you be able to see how thick the apical myocardium is. Use atypical apical views and a 2-chamber view to avoid foreshortening
5) Not using strain to assess hypertrophy
2D echo allows us to detect and measure the thickness on the myocardium. But a thick myocardium can mean many things. Does the patient have hypertrophic cardiomyopathy? Is it true hypertrophy what makes the septum thick or does the patient have a storage disease? This is where speckle tracking echocardiography comes into play. It provided information on the contractility of the myocardium and the strain pattern can help in the differential diagnosis of LVHMy Tip: Embark on the journey to learn speckle tracking echocardiography and use it in patients with LVH
Certainly there are many more teaching points to talk about when it comes to left ventricular hypertrophy. Let us know if there are any important topics you want us to cover!
For those of you who want to dig deeper we have much more teaching content:
https://www.123sonography.com/out-of-the-storm
Best Thomas Binder and the 123sonography team