Common mistakes - Diastolic Dysfunction
Did you ever take the time to read an old cardiology journal - maybe, one from the late 80ies – early 90ies? In a way, it is amazing how much we already knew about diastolic dysfunction 30-40 years ago. But then again it is also disturbing to see how so many recommendations never made it to clinical practice or have now vanished from the guidelines.
Certainly the medical community has learned from its mistakes. These together with my personal failures in the assessment of diastolic dysfunction are the topic here. So what should we avoid doing?
1) To think that correct assessment of diastolic dysfunction is just a matter of using the available echo parameters.
What we all have learned over the years is that echo does not allow us to accurately assess the various components of diastolic dysfunction and that it is often difficult to put a stamp on the severity of “diastolic heart failure”. It might work better in some patients than in other. But the truth is: we simply don’t have a non-invasive parameter of chamber stiffness and it is impossible to discerned this component of diastolic dysfunction from elevated filling pressures related to other causes (such as systolic heart failure). This acknowledgement is also the reason why the societies are moving away from strict classification- and grading schemes to a decision trees where you will often end up with the result: “diastolic dysfunction undetermined”.My Tip: Don’t be frustrated if you are not able to provide the answer. Better no conclusion, than a wrong conclusion.
2) To think that HFpEF is “diastolic heart failure”
At least that’s what I thought until Speckle Tracking Echocardiography came along and thought me that many patients with heart failure and normal ejection fraction actually have a reduction in systolic strain. Strain is much more sensitive than ejection fraction. Most patients with HFpEF have a combination of diastolic AND systolic dysfunction.My Tip: Use strain, use strain, use STRAIN!
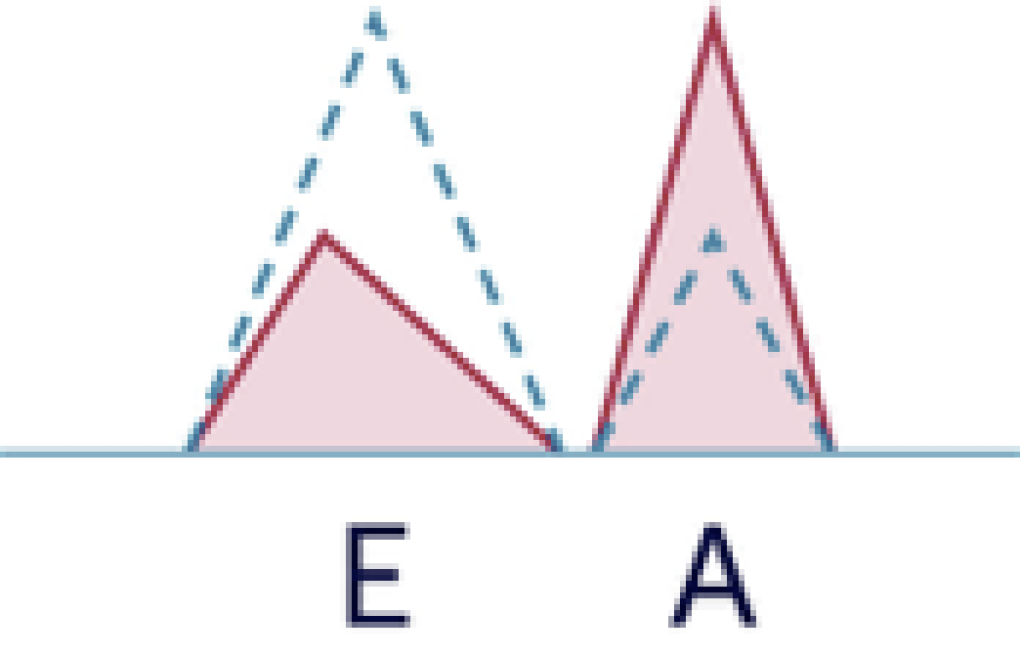
3) Mixing up the A wave with an “L-wave”
The A wave can be truncated (cut off by the contraction of the ventricle) - especially if the AV (PQ interval) is short (or set short in pacemaker patients). If patients also have an underlying condition such as a low heart rate and diastolic dysfunction (as in LVH HCMP, CAD) they might also have an “L-wave” (mid-diastolic flow across the mitral valve). In such situations you might think that the L wave is the A wave. By prolonging the AV time (pacemaker) you will be able to detect the true A wave and tell that what you thought was the A wave was actually the L wave.My Tip: look at several beats. Prolong the AV time on pacemakers. If you have an L wave you already made the diagnosis that filling pressures are elevated and that diastolic dysfunction is present
4) Not putting your findings into a clinical context.
There are so many factors that influence parameters of diastolic dysfunction. This makes the interpretation so difficult. But be aware that no matter which conclusion you draw it has to fit into the clinical context and into the overall pattern of your other findings. For example: a patient with severely reduced LVF cannot have “normal” diastolic function”. The same is true for patients with severe LVH, mitral regurgitation, severe aortic stenosis and many other conditions.My Tip: The 2D image is key to interpreting diastolic function. Look at the size of the left atrium, left ventricular function, the presence of mitral regurgitation, LVH etc. All of these findings affect or can be the cause of diastolic function
5) Using E/e´ to estimate filling pressures
True, there is a smart theory behind using E/e´ to assess filling pressures. However, many of these assumptions are based on observational data. For example that e velocity is inversely related to tau (the most established index to describe left ventricular diastolic function). But, while you might find a relationship between E/e´ and filling pressures in a large cohort this is not always true in individual patients. There are just too many factors that also affect the E/e´ ratio. I recall many patients in whom I was certain that their filling pressure is elevated, still E/e´ was normal and vice versa.My Tip: Use E/e´ only as one parameter of many to assess diastolic dysfunction. Learn to correlate E/e´ with the symptoms (dyspnea) of the patient.
The bottom line of my learning’s over the years related to diastolic function:
Best Thomas Binder and the 123sonography team