12.7 Quantification of mitral regurgitation
With echocardiography it is easy to detect mitral regurgitation. In contrast, quantification of mitral regurgitation is much more difficult. It calls for considerable experience. No single method or feature can be used to fully describe the severity of mitral regurgitation. All components of quantification must be considered; an integral approach should be adopted. In addition, it is important to understand the hemodynamics and sequelae of mitral regurgitation. Put all the pieces of the puzzle together and interpret your findings in the context of clinical findings. Ultimately, the severity of mitral regurgitation determines whether one opts for a surgical, an interventional (e.g. the MitraClip procedure) or a conservative approach.
| Qualitative (visual assessment) | Semiquantitative | Quantitative |
|---|---|---|
| Jet size (vena contracta, flow convergence) | Size of vena contracta | PISA method |
| LV size (and function), LV volume overload? | Size of flow convergence zone | Volumetric method |
| PA pressure | Jet area | |
| (MV morphology) | ||
| (left atrial size) | ||
| (other indirect signs) |
12.7.1 The mitral regurgitation jet
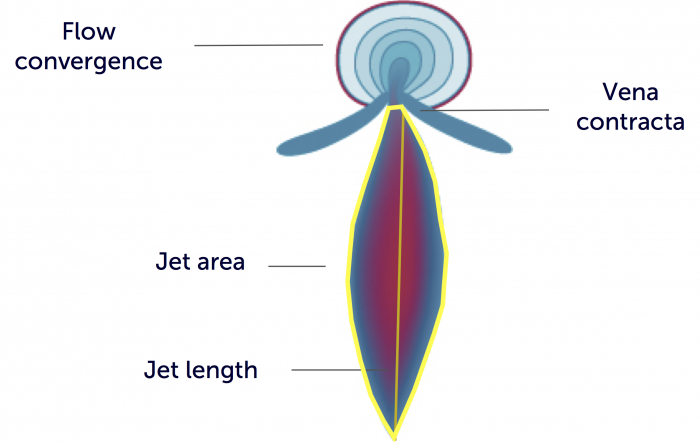
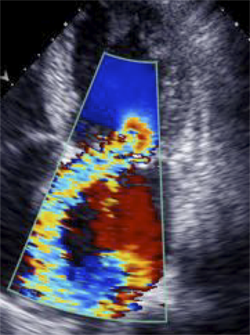
Color Doppler is able to directly display the high velocity "backflow" of blood into the left atrium in form of a "jet". The "dominant" color of the jet corresponds to the direction of flow (red to, and blue away from, the transducer). As velocities in such jets exceed the Nyquist limit and because of turbulent flow (see Chapter 1 Principles of echocardiography), there will also be an array of other colors in the jet. It is this "aliased" flow that makes jets easily visible. In general, the larger the jets are, the more regurgitation is present. How does one quantify the size of a jet? What factors, aside from the degree of regurgitation, influence the way a jet is displayed? To answer these questions we first have to look at the various components of a jet:
Mitral regurgitation is a dynamic process; the magnitude of regurgitation differs in early, mid, and late systole.
Flow convergence zone: The flow convergence zone is the zone of increased flow velocity before the regurgitant orifice, just as the flow of water in a river increases prior to a rapid. Another analogy would be the swirls of water one sees in a bathtub close to the outlet. The velocity of flow increases towards the regurgitant orifice in concentric shells, causing a more or less semicircular region of aliased flow. The size of this region corresponds to the magnitude of blood flow and the size of the regurgitant orifice. Thus, it can be used to quantify the severity of regurgitation.
The flow convergence zone is probably the most important part of the jet when it comes to quantifying regurgitation. "Visual assessment" of the severity of mitral regurgitation is based on the flow convergence zone. It may also be used to directly measure the volume of regurgitation and the effective regurgitant orifice area with the aid of the PISA method (see below).
It is quite difficult to quantify the size of the flow convergence zone. Quantification methods solely based on actual measurements have several limitations (these will be discussed in the section on the PISA method). However, one may use a crude semiquantitative scale: Trivial or mild forms of regurgitation are characterized by the absence of a flow convergence zone (too small to be detected with echo). In moderate forms the flow convergence zone will be visible but small (<4). In severe forms it will exceed 1.0.
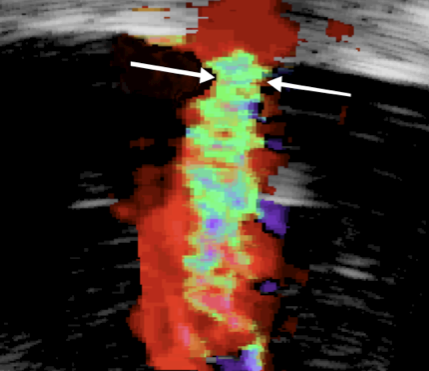
Vena contracta: The vena contracta corresponds to the region in which blood passes through the valve. Velocity is highest here. The width of the vena contracta is a good marker of the severity of mitral regurgitation because it corresponds to the diameter of the regurgitant orifice area. A diameter exceeding 7 mm indicates severe regurgitation. However, like all distance measurements it is limited by two facts: a) regurgitant orifices may have many geometric shapes, b) quite often more than one jet is present. Nevertheless, the vena contracta is an important clue to the severity of regurgitation.
Jet body: The portion of the jet that is seen in the "receiving camber" (the left atrium) is the "jet body". Its size also corresponds to the severity of mitral regurgitation. Several methods of quantification have been proposed, including jet area and jet length. However, none of these parameters are reliable because they are strongly dependent on color gain and color aliasing settings. Specifically, the length of the jet and whether or not it reaches the roof of the left atrium are no good markers of severity. Other proposed methods, such as jet area or the relationship between jet area and the left atrium are more accurate. Yet, none of these parameters can be used alone to quantify regurgitation. These methods lead to underestimation of severity in eccentric jets because they are prone to the "Coanda effect", in which the jet impinges the left atrial wall. A part of the jet energy is lost and the jet appears to be smaller.
Beware of optical illusions: Relate the size of the jet to the size of the left atrium. In large atria the jet may appear smaller than it is.
The severity of mitral regurgitation is also influenced by the driving pressure of the left ventricle. Hypertension, for instance, may increase the degree of regurgitation.
Poor imaging of the jet is the greatest source of error in quantifying regurgitation.
| Mild | Moderate | Severe | |
|---|---|---|---|
| Vena contracta (mm) | < 3 | 3—6.9 | ≥ 7 |
| Jet area (%) | Small central jet (<20% of LA area) | Variable | Large central jet (%gt;40% of LA area) |
In summary, the jet and its components permit a qualitative as well as semiquantitative approach to quantification. Regurgitation is usually graded as trivial/mild, moderate or severe. Although this approach is quite subjective and has several limitations, it works well and still is the most widely used method. In fact, there is widespread agreement among experienced investigators in this regard. The following examples provide templates for quantification.
Trace MR
Mild MR
Severe MR
12.7.2 Imaging of the jet
Every jet looks different. Its origin, direction and magnitude may vary considerably. Besides, more than one jet may be present. Thus, all segments of the valve must be visualized when imaging regurgitation. Use a sweep technique to search for jets, and display their full extent with atypical views as well. Optimize the 2D image before you use color Doppler because poor image quality in 2D will lead to poor Doppler quality.
The way a jet is displayed also depends on the angle of insonation. Centrally directed jets will not be adequately displayed from a parasternal long-axis view. Therefore, use a transducer position that is as parallel as possible to the jet. Several orthogonal views will be needed to appreciate the shape and three-dimensionality of a jet. For this purpose, rotate the transducer around the axis of the jet.
Imaging should be tailored to the jet - not to standard views.
As mentioned earlier, imaging should focus on proximal portions of the jet, the flow convergence zone, and the vena contracta. In certain settings (e.g. bi-leaflet mitral valve prolapse regurgitation), regurgitation is not holo- but mid to late systolic. This may also lead to overestimation of its severity.
To display the timing of regurgitation use CW Doppler through the jet
12.7.4 Volumetric method
The volume of regurgitation is calculated as the difference between transmitral flow and flow across the left ventricular outflow tract LVOT).

Principle of volumetric calculation
The fraction for calculation is:
RF (%) = (MV regurgitant volume / Transmitral volume) x 100
Flow is calculated in the same manner as stroke volume (see Chapter 3); the velocity time integral (PW Doppler) is multiplied by area (Area = π . (D/2)2). For systemic flow this is usually done at the left ventricular outflow tract. Flow calculations across the mitral valve are performed at the mitral valve (annulus of the mitral valve on a four-chamber view). In theory this approach is quite appealing. In clinical practice, however, it does not work well. First, the mitral valve is by no means round. Thus, its size cannot be calculated from its diameter. Secondly, it cannot be used when aortic regurgitation is present.
Regurgitant fraction can also be calculated by using regurgitant volume derived with the PISA method.
Reference values for the different degrees of regurgitation are presented in the following table:
| Mild | Moderate | Severe | |
|---|---|---|---|
| Regurgitant Fraction (%) | < 30 | 30—39, 40—49 | ≥ 50 |
12.7.5 Retrograde flow in the pulmonary veins
The flow pattern in the pulmonary veins is altered in mitral regurgitation. Two factors are responsible for this change: a) left atrial pressure is elevated, and b) reverse flow into the left atrium occurs during systole. This causes either blunted or reverse systolic flow in the pulmonary veins. The flow pattern in the pulmonary veins may also be used to quantify the severity of mitral regurgitation.
| Retrograde flow in pulmonary veins | ||
|---|---|---|
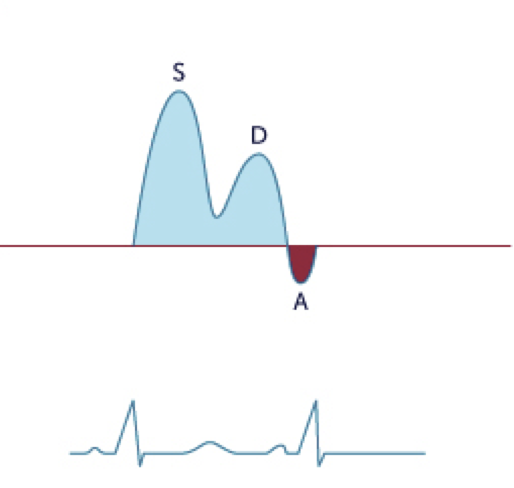 | 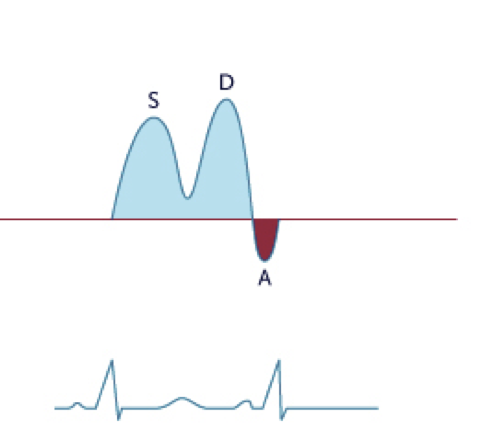 | 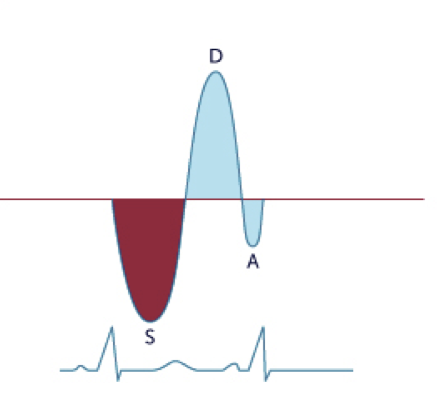 |
| Normal flow | Blunted flow | Systolic flow reversal |
However, interpretations must be made with caution because the method has several limitations:
- It may be difficult to obtain tracings of good quality.
- The direction of the jet (i.e. into the right pulmonary artery) may affect the signal.
- Other causes of elevated pressure in the left atrium (i.e. diastolic dysfunction, left ventricular dysfunction, atrial fibrillation) may cause blunted flow.
- Interpretation is difficult in the presence of atrial fibrillation.
One rarely needs to assess the pulmonary vein in order to determine the severity of mitral regurgitation.
12.7.3 The PISA method
The PISA (proximal isovelocity surface area) method employs the proximal flow convergence zone to measure the volume of regurgitation
PISA is also a city in Italy....
The principle underlying this method is straightforward: the flow convergence zone corresponds to regurgitant flow. Blood flow velocity increases as it approaches the regurgitant orifice. The proximal flow convergence zone can thus be described as "hemispheric shells" in which the velocity on the surface of each of the shells is equal. The quantity of blood flow (regurgitant flow) can be calculated when the radius of the shell and velocity at its surface are known:
Regurgitant flow = Q = 2 x r2 x π x Nyquist vel.
With the PISA method we use the shell where aliasing occurs - where the color abruptly switches from a distinct blue or red to turbulent (multicolored) flow. Velocity (aliasing velocity) can be determined exactly at this site. We can also measure the radius (r) of the hemisphere at this site.
EROA = [(2r2 x Vpisa)/ Vmr]
Based on the principle of conservation of mass, the PISA method also permits us to measure the effective regurgitant orifice (the functional size of the "hole"). To perform this calculation we have to know the peak velocity of the MR signal. This is achieved by obtaining a CW Doppler spectrum through the mitral regurgitant jet.
Limitations of the PISA method
The PISA method has been validated in many studies, but still has numerous limitations that need to be addressed:
- The regurgitant orifice is rarely round. Thus the PISA is not a perfect hemisphere.
- Jets which are eccentric in origin demonstrate a PISA that is not hemispherical.
- Motion of the annulus during systole influences the calculation.
- Measurement of the PISA radius is difficult.
- Alignment with the direction of flow is sometimes impossible.
- Multiple jets are usually present.
- Regurgitation is usually dynamic. Thus, the mid-systolic frame might not be representative of MR.
- The method cannot be used in calcified and prosthetic valves.
Some of these issues are currently addressed with 3D echocardiography, which has been able to circumvent the problems related to the true shape of the PISA. At present all of these limitations must be considered when using the PISA concept. The calculations should always be viewed in conjunction with other findings.
A semiquantitative approach: looking at the PISA is usually sufficient.
From a practical perspective you first need to first visualize the flow convergence area. Then adjust the aliasing limit to a value between 20-40 cm/s, and shift the baseline downward. This will give you a larger hemisphere, which facilitates measurement. Measurements should be performed at mid-systole. Freeze the image and measure the radius from the leaflets to the dome of the PISA. To measure MR velocity, obtain a CW Doppler tracing through the jet and trace the contour. This will also yield the peak velocity. As the PISA formula is included in the measurement program of most scanners, the calculations are performed automatically. Reference values for mild, moderate and severe mitral regurgitation are shown in the following table:
| Mild | Moderate | Severe | |
|---|---|---|---|
| PISA Radius | <0.4 | >1.0 | |
| Regurgitant volume (ml/beat) | <30 | 30—44. 45—59 | ≥ 60 |
| EROA (cm2) | <0.2 | 0.2—0.29. 0.3—0.39 | ≥ 0.4 |
12.7.6 Associated findings in mitral regurgitation
Moderate to severe mitral regurgitation also has an impact on the chambers and function of the heart. The size and function of the left ventricle are indicators of the severity of MR. Expect to see the typical signs of left ventricular volume overload (dilation and supranormal function) in the presence of significant regurgitation. Besides, the left atrium will be enlarged. However, its size cannot be used to quantify the severity of mitral regurgitation because it also depends on the compliance of the left atrium, the presence of atrial fibrillation, diastolic dysfunction, and other aspects. Another factor to look for is pulmonary pressure. Mitral regurgitation is relevant when pulmonary pressure is high (in the absence of other causes of pulmonary hypertension). In addition, pulmonary hypertension correlates well with symptoms, and may indicate "decompensated" mitral regurgitation. Conversely, the absence of pulmonary hypertension does not exclude severe mitral regurgitation. All of these findings must be monitored closely because they are linked to the treatment strategy. Other common features include bulging of the interatrial septum to the "right", and dilated pulmonary veins. Both of these phenomena result from increased left atrial pressure and atrial volume overload.
Associated findings:
- Dilated LV
- Hyperdynamic LVF
- Elevated mitral inflow velocity
- LA enlargement
- IAS bulging (towards RA)
- Dilated pulmonary veins
- Pulmonary hypertension