Paradox Endocarditis
Did you catch the pathology, which is responsible for bilateral pneumonia and the systolic murmur of the patient with endocarditis in our last post?
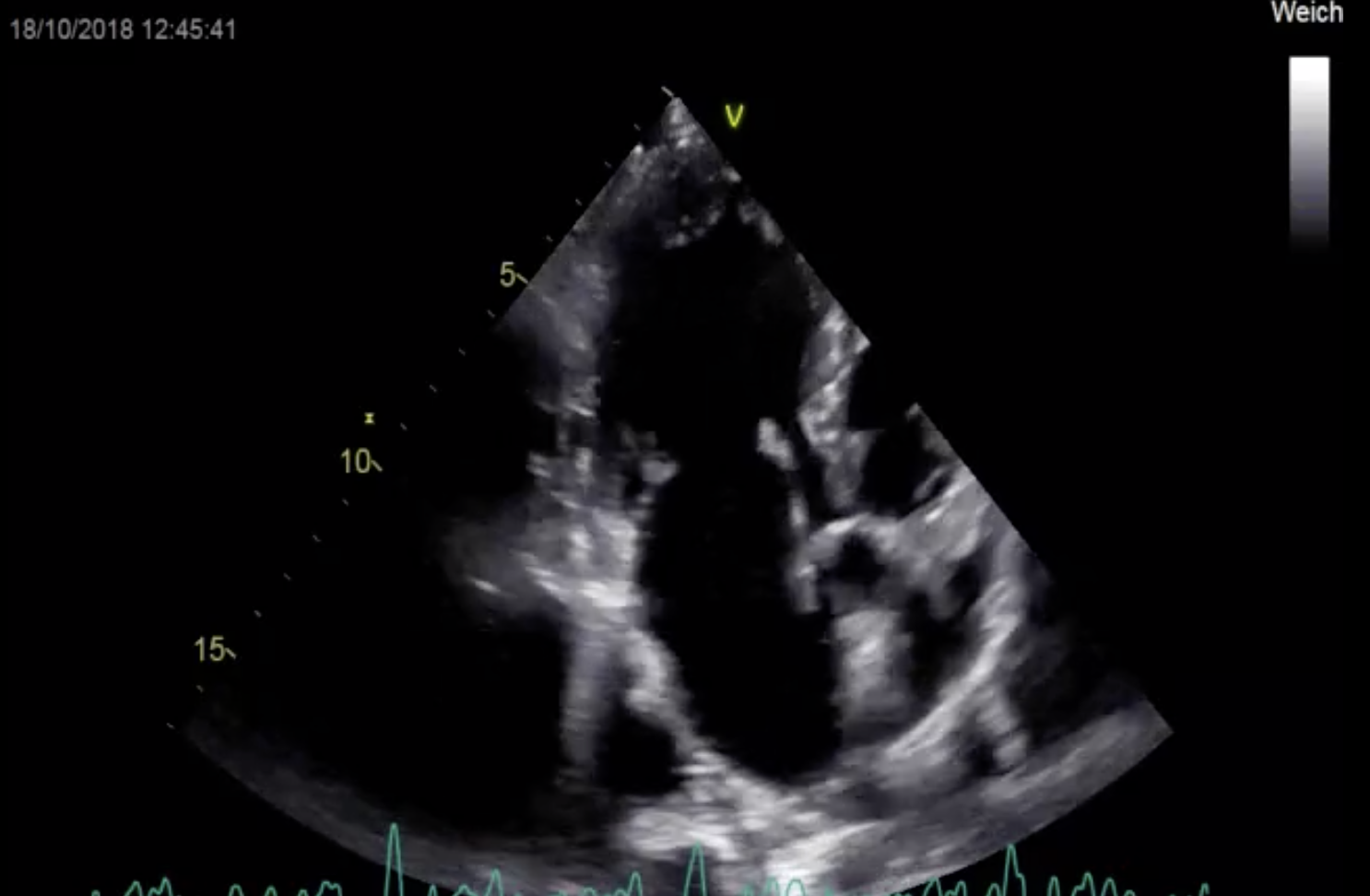
Here is the image that provides the clue:
Apical long axis view demonstrating endocarditis of the aortic- and mitral valve and an aneurysmatic VSD
The patient has vegetations on both the mitral and aortic valve. But did you also catch the strange appearance of the basal interventricular septum? We call this pathology a “perimembranous aneurysmatic VSD”.
What is an aneurysmatic VSD?
A ventricular septal defect (VSD) occurs in about 2-6 of 1000 births. In most situations, the VSD is rather small and restrictive. Over time these small defects can be either completely or partially covered by tissue that arises from the margins of the defect and the septal leaflet of the tricuspid valve. Let us take a closer look:
Zoom view of the LVOT outflow tract and the membranous interventricular septum in a 5 chamber view. The aneurysmatic transformation of the VSD is clearly visible.
You can see the defect in the membranous part of the interventricular septum and the tissue, which gives the structure an aneurysmatic appearance. The defect is best visible in a 5 chamber view, but can also be seen in an apical view and with transesophageal echo.
TEE long axis view displays the defect in the basal interventricualar septum. Note how close the defect is to the aortic valve.
To detect the defect with TEE it is important to rotate the probe back and forth so that the area of the aneurysmatic transformation is visible. Note how the aneurysm extends into the right ventricle. Such aneurysms can actually get quite large. When evaluating such an aneurysmatic VSD be sure to exclude a thrombus. A few such cases have been described in the literature.
Complete or incomplete?
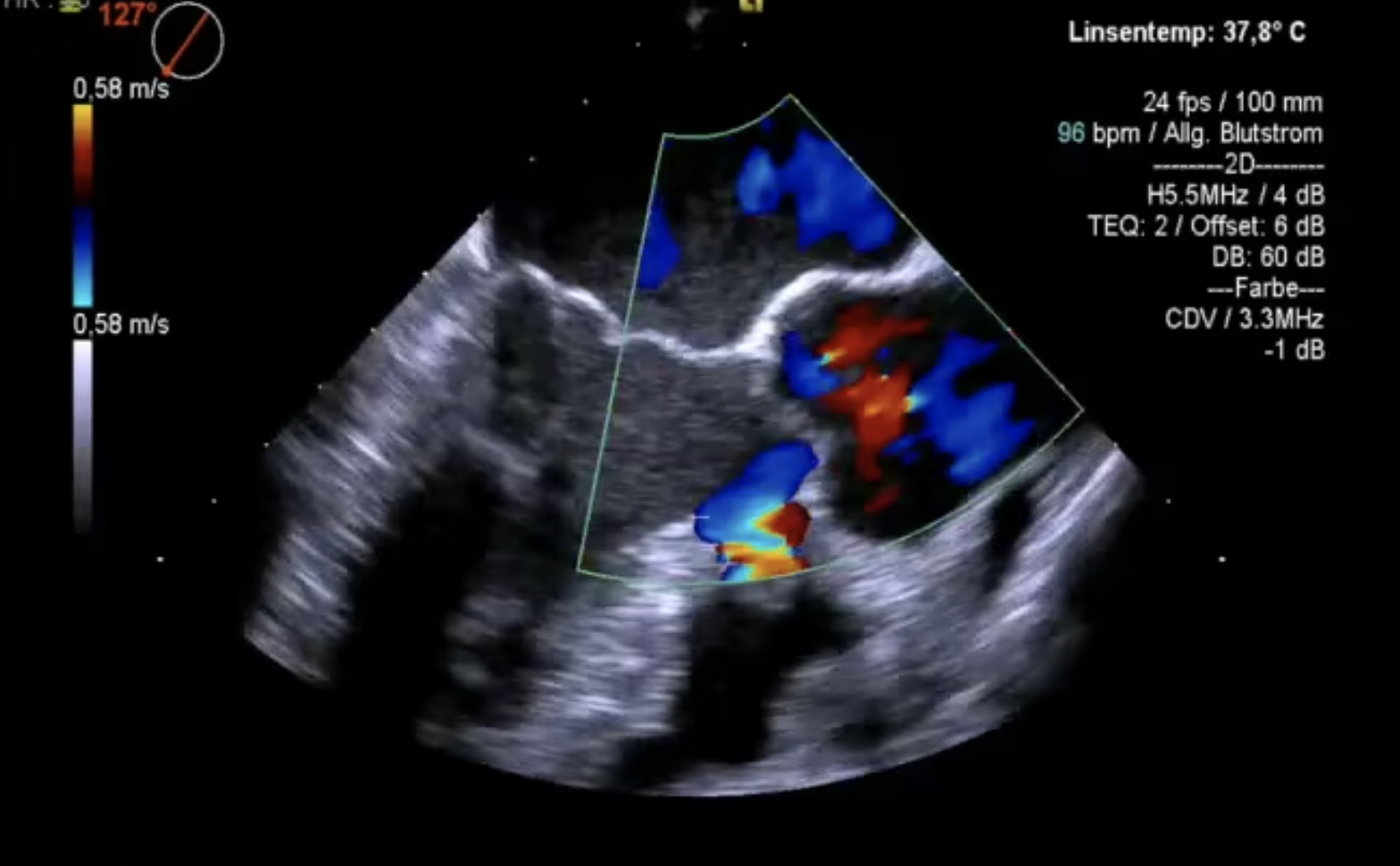
There is only one more open question: Is the VSD completely or only partially sealed? Color Doppler provides the answer:
TEE long axis view demonstrating a residual VSD
Now we have the explanation for the murmur and also an explanation why the patient has bilateral pneumonia. Here is the sequence of events:
The patient was born with a VSD and has mild mitral valve prolapse, which predispose to endocarditis. The valve, which was primarily infected, was most likely the mitral valve. Infection then spread to the aortic valve and via the VSD to the lungs where it caused bilateral pneumonia. In analogy to paradox embolism we might call this a case of “paradox endocarditis”.
Teaching points:
There are three main teaching points from this case:
- Always expect the unexpected in every patient and think outside the box
- Patients with a VSD are at higher risk (six fold) for endocarditis
- Some times all you need to become a hero is a stethoscope
Best Matthias Schneider, Thomas Binder and the 123sonography team