PCOS: Navigating the Controversies – What Should We Focus On?
September is Awareness Month for several OB/GYN topics, including PCOS Awareness Month. Polycystic Ovary Syndrome (PCOS) is a term that has become familiar to both healthcare professionals and patients. As the most common endocrine disorder in women of reproductive age, it has sparked significant debate, particularly regarding its diagnostic criteria.
The Rotterdam Criteria: Strengths and Limitations
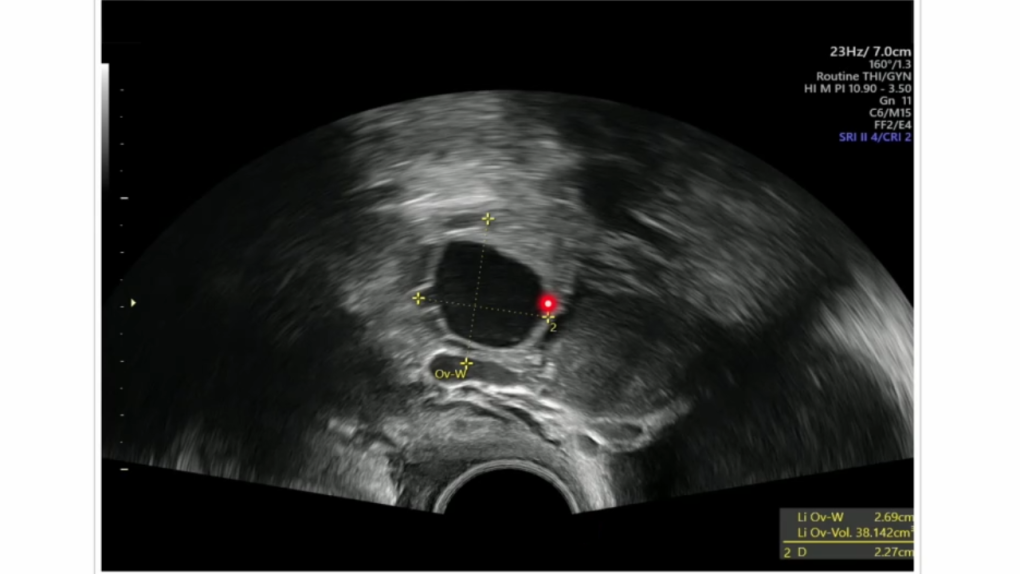
The Rotterdam criteria, established in 2003, are the most widely accepted for diagnosing PCOS. They define the presence of Polycystic Ovarian Morphology (PCOM) as one of the three key diagnostic features, alongside hyperandrogenism and ovulatory dysfunction. According to these criteria, PCOM is identified when there are 12 or more follicles measuring 2-9 mm in size throughout the ovary or when the ovarian volume is greater than or equal to 10 cm³.
However, the inclusion of PCOM as a diagnostic criterion is not without controversy. The original thresholds were based on a single study comparing women with PCOS to controls. Since then, significant advances in ultrasound technology, operator variability, and lack of standardisation have highlighted the limitations of the Rotterdam criteria. Moreover, these criteria do not account for factors such as age, body habitus, and the type of ultrasound approach used, all of which can affect the appearance of the ovaries.
The Adolescent Conundrum: PCOM in the Young
One of the most debated aspects of the Rotterdam criteria is their application in adolescents. During the early years after menarche (up to eight years post-menarche), multi-follicular ovaries are often a normal finding. Therefore, diagnosing PCOS in adolescents based solely on ultrasound findings of PCOM can lead to overdiagnosis.
Studies have shown that up to 70% of adolescents meet the Rotterdam criteria for PCOM, yet this does not correlate with reproductive dysfunction. The term “polycystic” is somewhat misleading, as it refers to arrested follicles rather than true cysts. This misinterpretation can result in unnecessary concern and inappropriate labelling of young women.
The natural fluctuation in antral follicle count during puberty and the early post-menarcheal years further complicates the picture. Given the significant overlap between normal ovarian morphology in adolescents and the PCOM seen in women with PCOS, it is clear that the adult criteria are not suitable for this younger population. In adolescents, PCOM should be considered alongside clinical signs of hyperandrogenism and ovulatory dysfunction rather than as a standalone diagnostic feature.
Moving Forward: What Can We Rely On?
Despite these controversies, there is good news. Most women with clinical and endocrinological features of PCOS do exhibit polycystic ovaries on ultrasound, which is why PCOM was included as a diagnostic criterion in the first place. However, caution is warranted when interpreting ultrasound findings in postmenarchal women, especially within the first eight years after menarche.
Ultrasound example:
While ultrasound remains an essential tool in screening for other pathologies, it should not be the sole determinant in diagnosing PCOS, particularly in adolescents. A more nuanced approach, considering the patient's age, clinical symptoms, and other diagnostic features, is necessary for accurate diagnosis and management.
In conclusion, as our understanding of PCOS evolves, so too must our diagnostic criteria. It is crucial to recognise the limitations of current methods, particularly in young women. By refining these criteria and ensuring they are applied judiciously, we can improve the accuracy of PCOS diagnoses and better support the women affected by this condition.
Learn more about ultrasound for PCOS but also other common pathologies in OB/GYN with our OB/GYN Ultrasound BachelorClass. Until September 20th, 2024, available with exclusive Lifetime Access and a 10% discount! Get course now!