Far From Home
Today I would like to report about a patient I saw several years ago in a “developing” country during a cardiac training program I attended.
The hospital staff and trainees were not only extremely friendly but also eager to learn more on newer technologies of ultrasound. Together with the local echo-team I saw a 48-year-old man who was just brought in from a remote area of that country. The patient had been admitted to the critical care unit of the hospital with bilateral pulmonary effusion and peripheral edema. According to his wife he had been suffering from dyspnea for quite some time.
The ECG showed atrial fibrillation and a wide QRS with left-bundle-branch-block (LBBB). At the time I saw him he was on mechanical ventilation, treated with diuretics and catecholamines and was more or less stable.
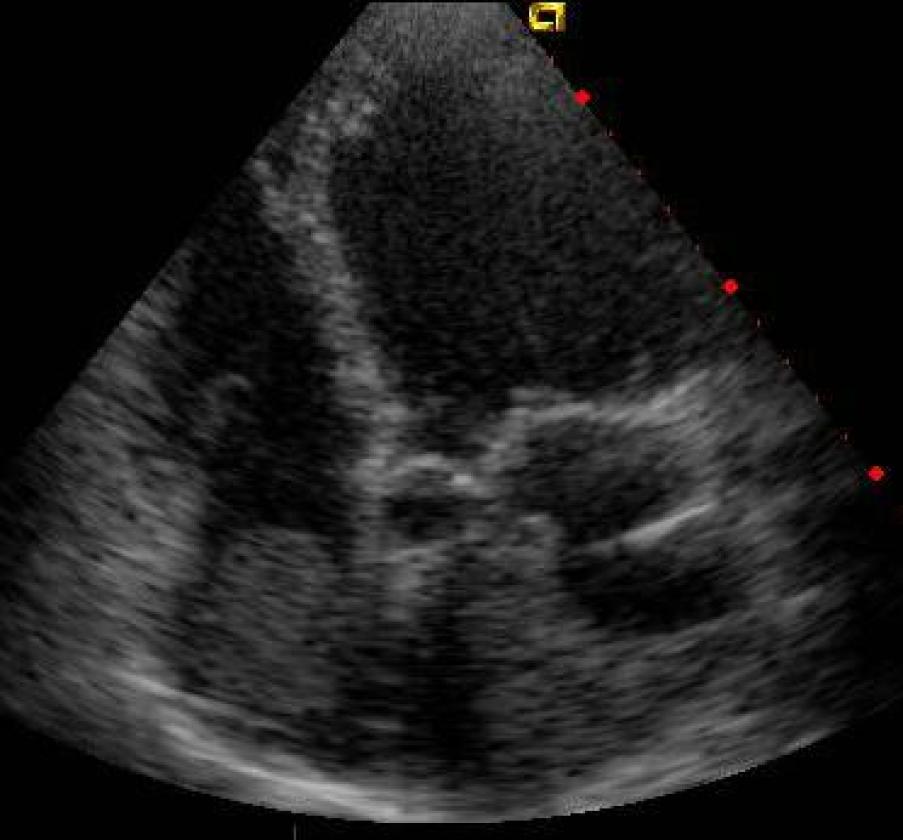
Here is the bed-side transthoracic echo of this patient. I am sure you can all see what his problem was:
 Image 1: Apical 4 chamber view
Image 1: Apical 4 chamber view
 Image 2: Apical 2 chamber view
Image 2: Apical 2 chamber view
 Image3: Atypical apical view
Image3: Atypical apical view
Both ventricles were dilatated and both left and right ventricular functions were severely reduced. In addition, there was a mass in the left and also in the right atrium. What do you think is the etiology of the mass? Well, my first question was, whether the patient had been anti-coagulated – a clear “No” was the answer!
Severely reduced ventricular function and atrial fibrillation had slowed down the blood-flow in the atria. This is a vicious combination, which strongly predisposes to thrombus formation. Note that the left and right atrium were almost completely filled with thrombotic masses.
No question, the patient needed anticoagulation urgently since he was at increased risk for both pulmonary and systemic embolism.
But anticoagulation would not have solved all his problems. It is clear that the patient had a poor prognosis whatever the reason for biventricular heart failure was. I was told the next day that he died the same night in cardiogenic shock and multiorgan failure.
We never found out what the cause of his heart problem was. Dilated cardiomyopathy? Myocarditis? Coronary artery disease? However, in the stage of the disease he was in, it probably didn’t matter. The only solution would have been urgent transplantation. But transplantation was simply not available in said country.
Why are we showing you this case?
Not only because it displays the rather rare finding of massive biatrial thrombi but also because it should remind us that reduced right ventricular function in the setting of cardiomyopathy strongly correlates with symptoms and is inevitably associated with a poor prognosis.
It also shows us that the risk of thrombi is especially high in patients with atrial fibrillation AND reduced ventricular function.
And finally, for all those who perform echocardiography on the intensive care or in an emergency setting - be reminded that transthoracic echo is feasible in many ventilated patients. All you need are the appropriate skills.
In order to learn those skills, visit us at www.123sonography.com!