Common mistakes - Left Ventricular Function
Are you familiar with the following scenario? You are imaging a patient where the EF that you calculate makes a huge difference. Will the patient be referred to surgery? Is heart failure treatment needed? Should chemotherapy be discontinued? How do you cope with such a situation and which mistakes should you avoid?
1) Focusing too much on ejection fraction
Forget “cut off values” for a minute. It is just as important to look at the size of the ventricle. Is it dilated? Is the LVOT velocity low? Are filling pressures elevated? What about pulmonary pressures? And finally, look at global longitudinal function (strain). All of these parameters together will help you understand how the patient is doing, what his prognosis is and what the best therapeutic option is.
Finding
Interpretation
LV very large
EF underestimates true function
LV very small
EF overestimates true function
Dyssynchrony
EF underestimates true function
Low LVOT vel. (<0.7m/s)
Low output syndrome, poor prognosis
Restrictive filling pattern, Elevated filling pressure
Decompensation , symptomatic
High sPAP
Decompensation, poor prognosis, symptomatic
Low global longitudinal strain
Poor prognosis, more sensitive than EF
A patient with an EF of 32% with normal sPAP, normal filling pressures and moderately reduced global longitudinal strain. The patient is completely asymptomatic.
My Tip: Learn to see the typical patterns of LV dysfunction and correlate them with the symptoms of the patient.
2) Foreshortening of the ventricle
If the transducer is not placed at the true apex you will miss out on an important part of the ventricle. Left ventricular volumes will be lower and EF will often be higher. Be aware that you do not get foreshortening in a 2-chamber view. If the LV is significantly longer in a 2 vs. a 4-chamber view than you should not perform a Simpson calculation of EF.
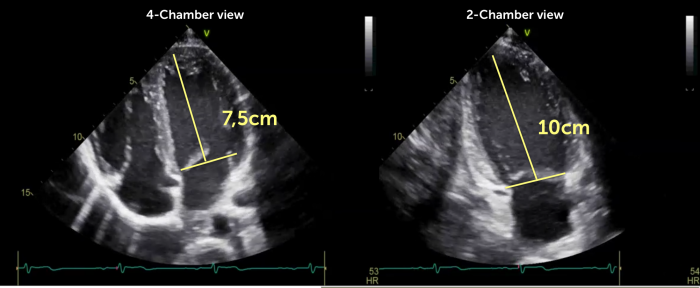 Example of foreshortening of the left ventricle in a 4-chamber view. The length of the LV in the 4-chamber view (7,5cm) is significantly less than in the 2-chamber view (10cm)
Example of foreshortening of the left ventricle in a 4-chamber view. The length of the LV in the 4-chamber view (7,5cm) is significantly less than in the 2-chamber view (10cm)
My Tip: Avoid foreshortening by moving the transducer more caudal. If this is not possible, be cautious when calculating EF
3) Tracing the wrong boarder
The inner lining of the left ventricle is far from smooth. If you look at the specimen of a heart you will see a crisscross of trebecula where the inner few millimeters have a rather spongy appearance. When tracing the endocardium you must focus on the compacted part of the endocardium. Otherwise your volumes will be too low.
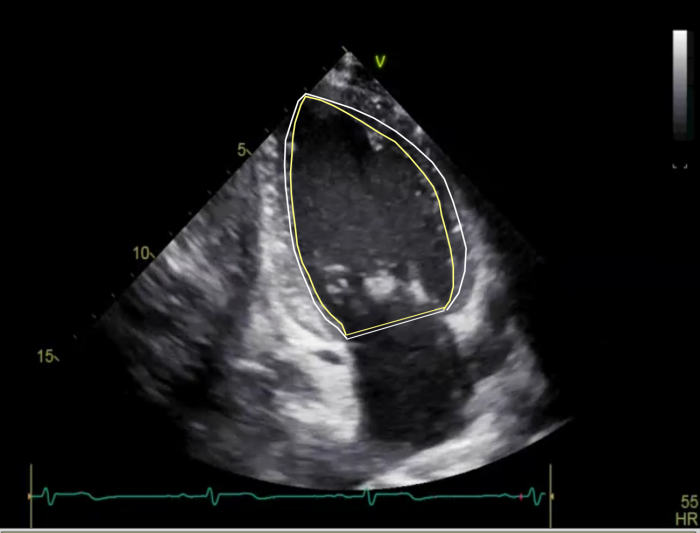 The endocardial boarder must be traced where the compacted layer is (white) and not at the inner lining of the trabeculations (yellow)
The endocardial boarder must be traced where the compacted layer is (white) and not at the inner lining of the trabeculations (yellow)
My Tip: Select a view where you can clearly see the compacted myocardium or use contrast
4) Overestimating LVF in small ventricles
A small ventricle (i.e. concentric LVH or hypertrophic cardiomyopathy) has to pump more vigorously to generate a sufficient stroke volume. So even if the ejection fraction is normal (or hyperdynamic) this does not mean that the ventricle is healthy. As a matter of fact we now know that many of these patients have a poor global longitudinal strain.
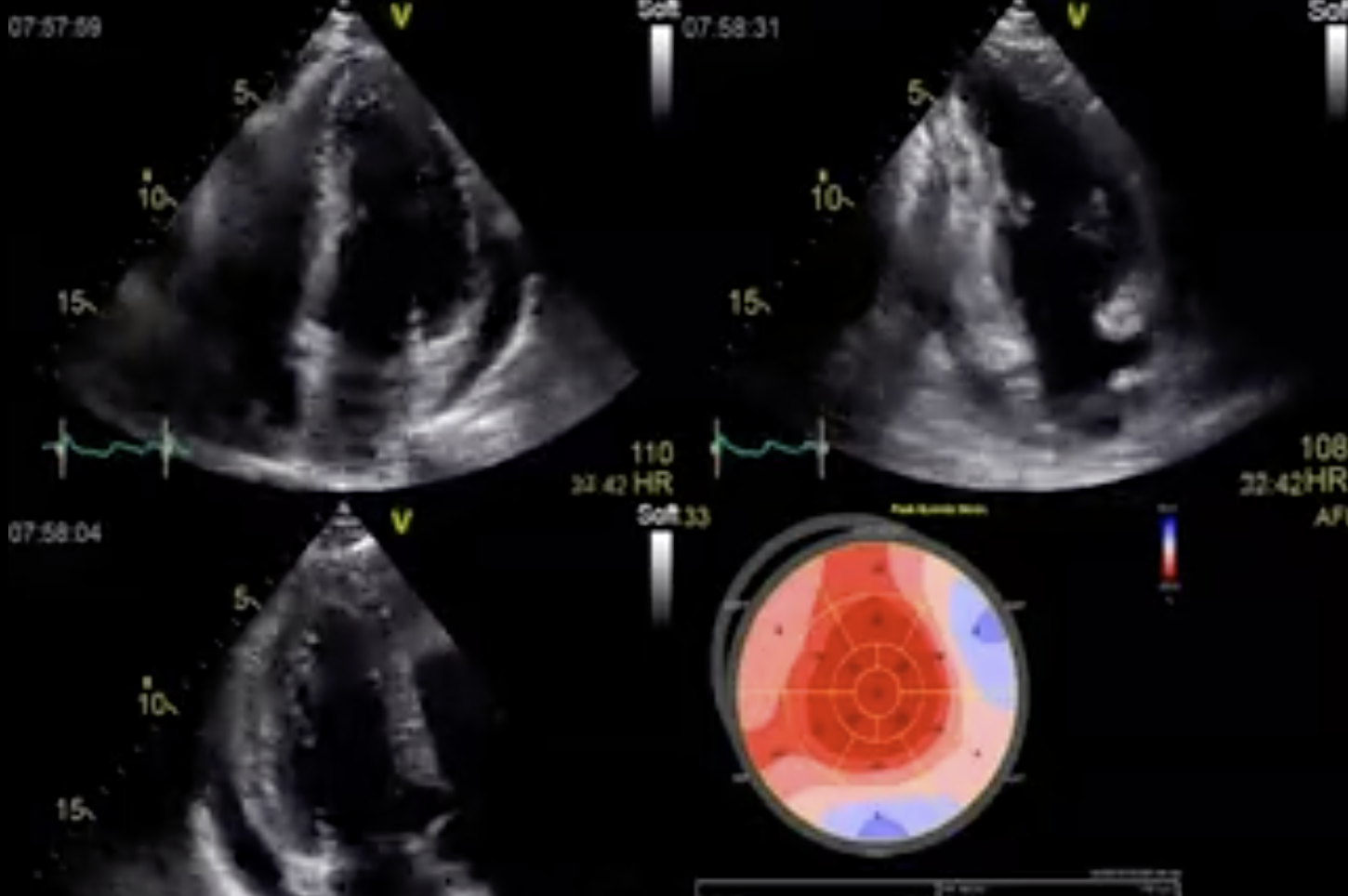
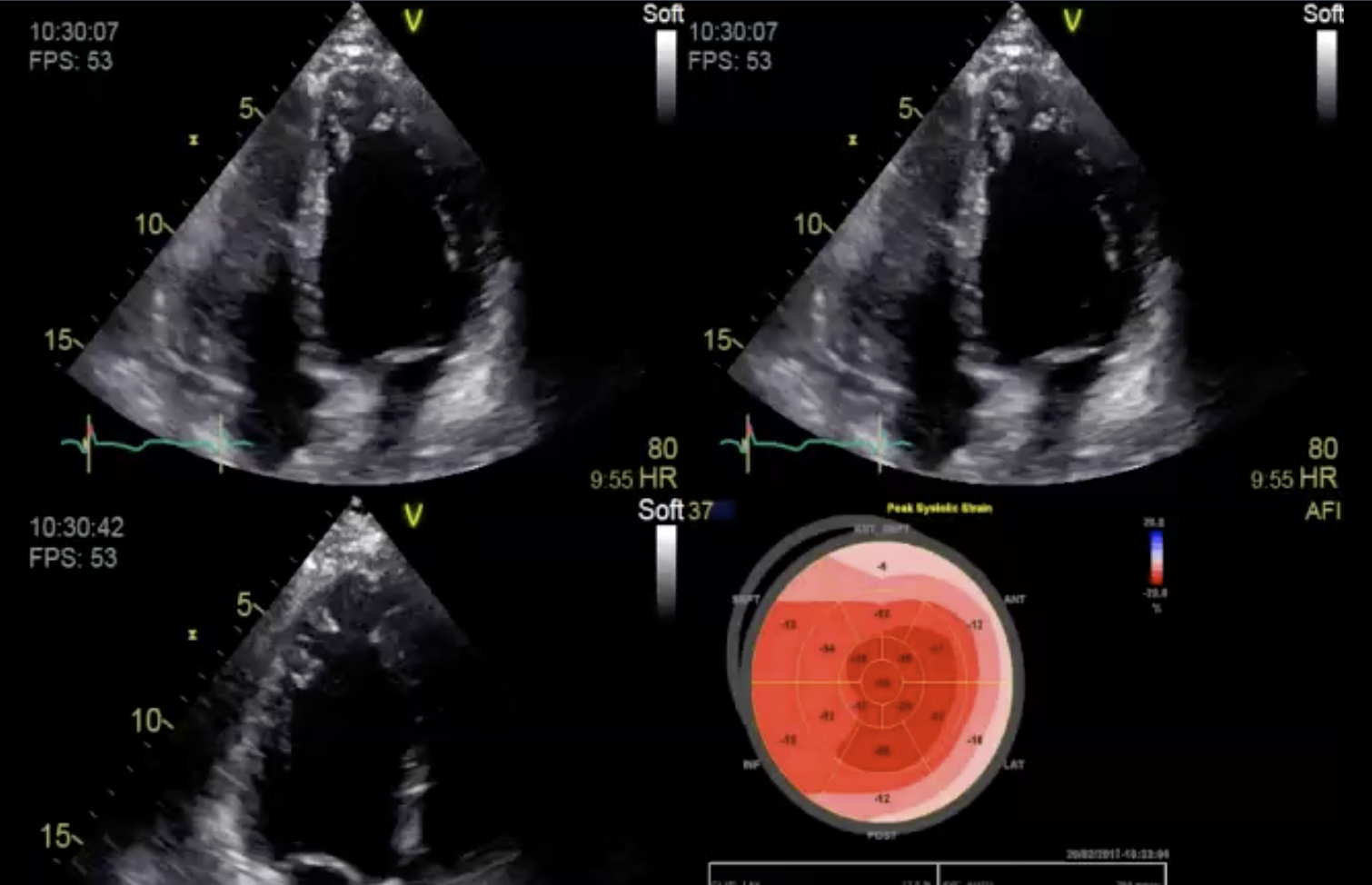
Example of a patient with a small left ventricle (hypertension / dialysis) and an EF of 76%. However, LVF is not normal as depicted by the significantly reduced global longitudinal strain (-9.2%)
My Tip: Perform a strain analysis and state in your report that the patient has left dysfunction despite a normal (or hyperdynamic) ejection fraction.
5) Apodictic believe in the numeric value of “ejection fraction”
Did you know that the measurement of ejection fraction can be off by 15%? The error is even larger if the observer is untrained or if the image quality is poor. Studies have also demonstrated that the mean beat-to-beat variation of ejection fraction in atrial fibrillation is 70%? This does not mean that you should not perform calculations of EF. But you will need to validate these measurements with your eye.
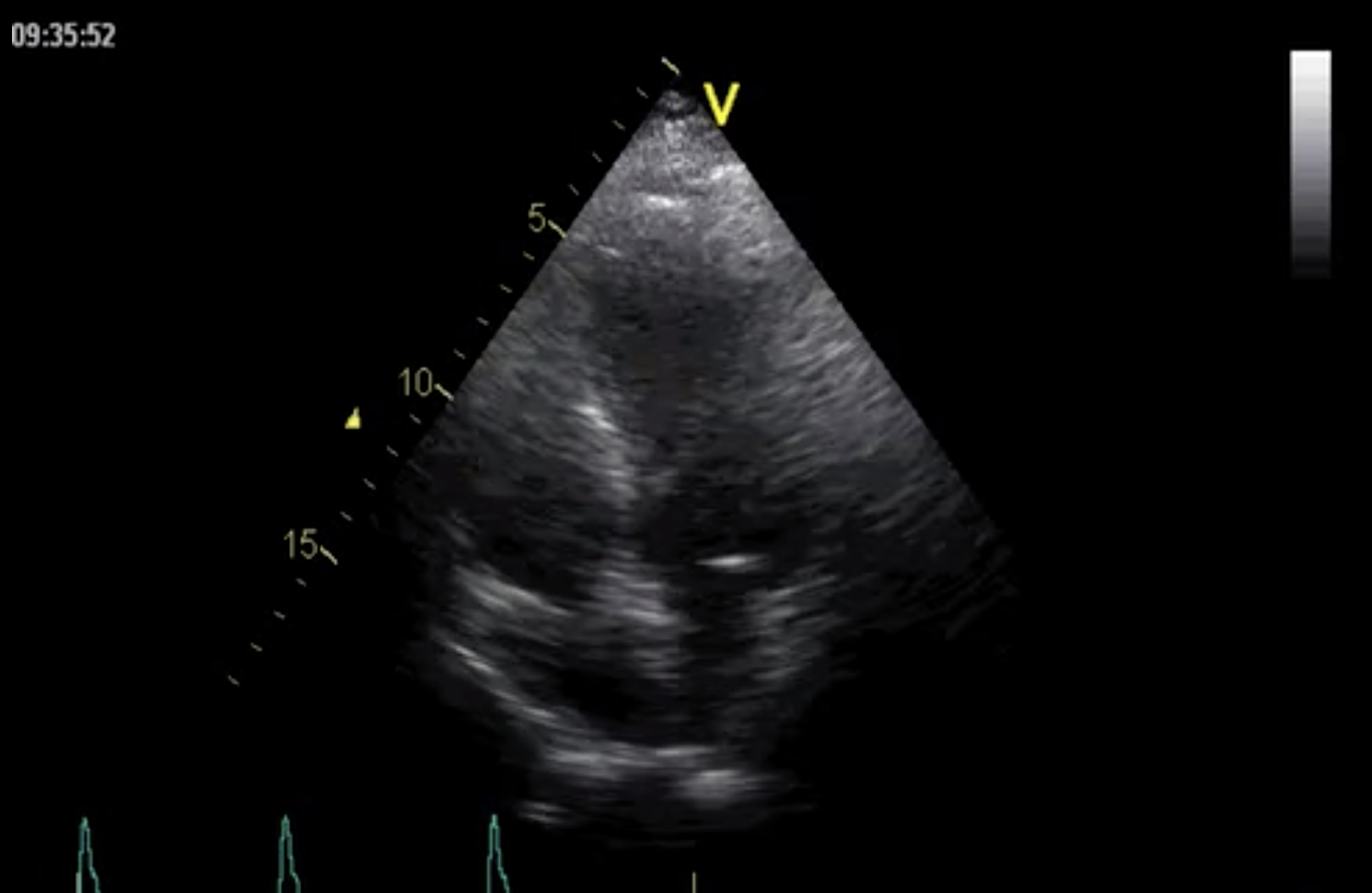
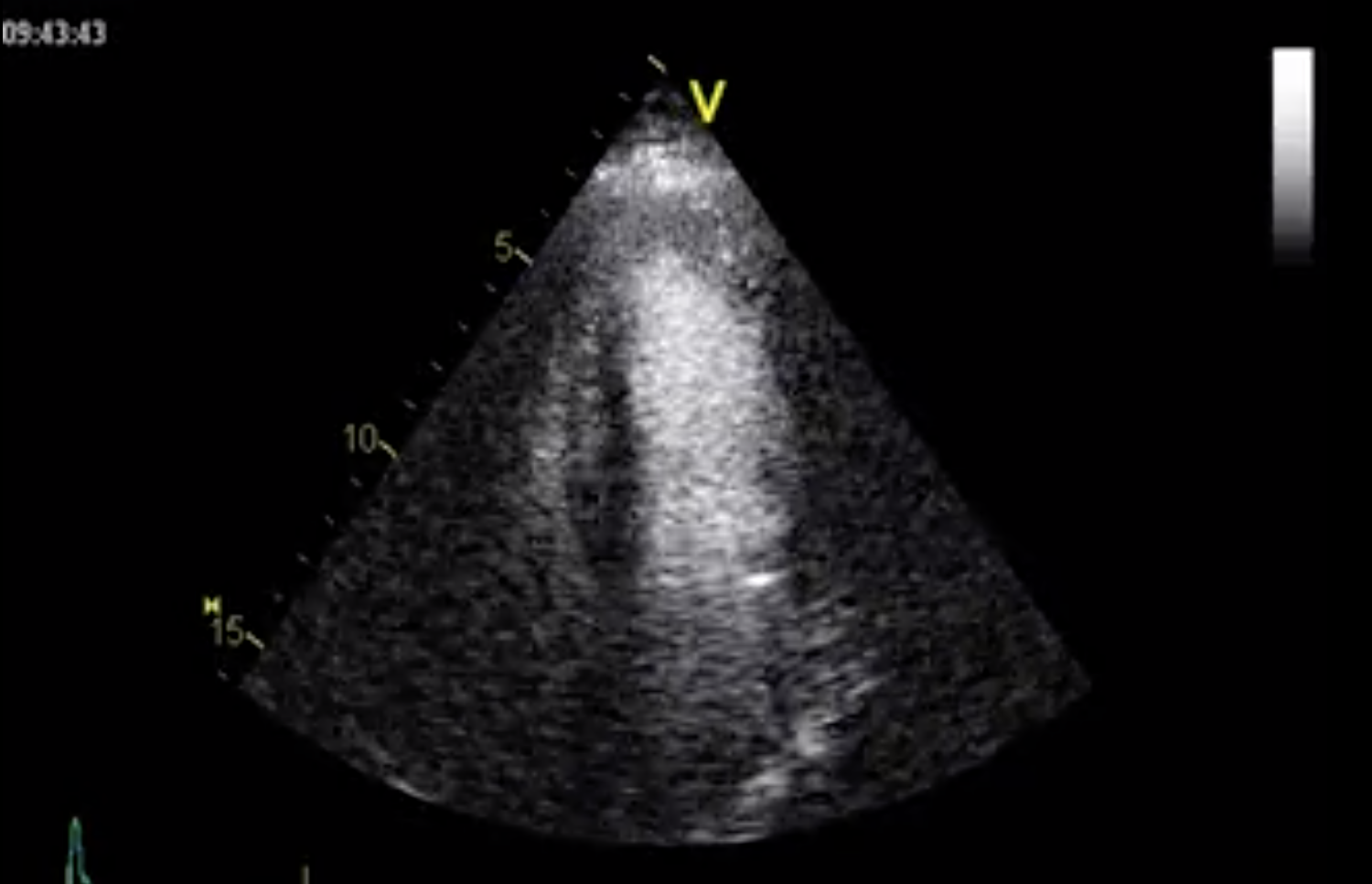
Poor image quality. It is not possible to assess or measure LVF correctly. Bei unterem Bild: Left ventricular contrast echo in the same patient. The ventricular cavity can now be clearly visible.
My Tip: Practice your visual assessment skills. Know the limitations of EF calculations and be skeptic. Use contrast in those settings where image quality is poor.
I hope my learnings are of value to you.
Best Thomas Binder and the 123sonography team