Common mistakes - Aortic Stenosis
As Albert Einstein put it:
Success comes from curiosity, concentration, perseverance and self criticism.
So lets jump right into some of the things that I learned by making mistakes. This time we will deal with the topic of aortic stenosis here are the top five:
1) You are focusing too little on the 2D image
Just because you record a high velocity does not mean the patient has aortic stenosis. There are several pitfalls: the high velocity is related to an LVOT obstruction (as in HCMP or subvalvular AS), you are seeing pressure recovery or you are actually measuring an MR signal. The degree of LVH is also importantit is not only associated with the severity of aortic stenosis (and the presence of hypertension).
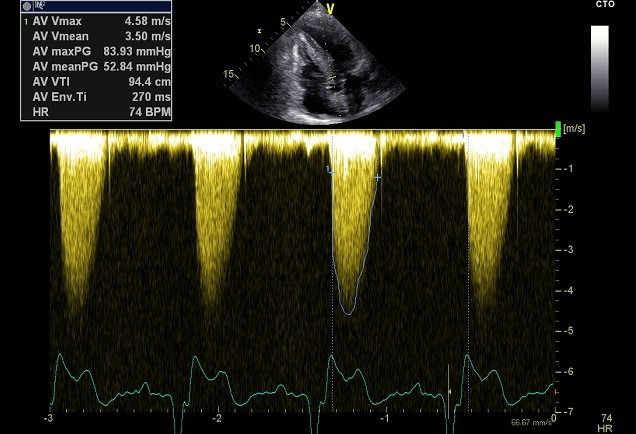
Example of a patient with subvalvular membranous aortic stenosis. The CW -Doppler velocity suggests severe aortic stenosis, however the aortic valve is not calcified and does not appear stenotic. The TEE study demonstrates a subvalvular membrane.
My tip: Look at the morphology of the valve, the shape of the signal, use color Doppler as a guidance and know exactly where your sample volume is placed
2) You are not using multiple views to measure the maximal velocity
Did you know that most patients with AS and bicuspid valves have eccentric jets? The classic 5-chamber view is often not the view where you would always get the highest velocity. Use different variations and also try from a right parasternal approach
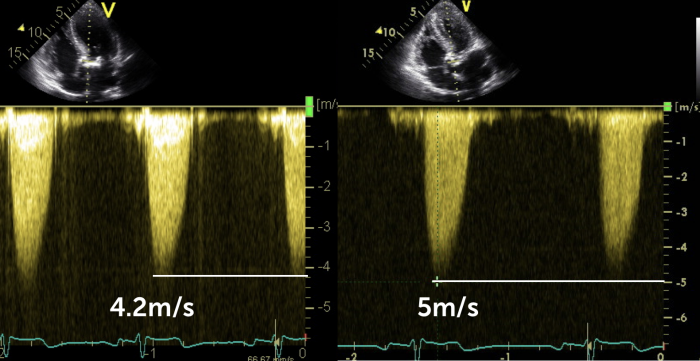
A slightly different orientation of the 5-chamber view when using CD-Doppler gives you a significantly different maximal velocity
My tip: Take your time when you look for the maximal gradients and try different transducer positions even within one view
3) You are extrapolating the measurements of maximal velocities
Sure, we want to get the highest possible velocity, but this is not a competiton. So do not over measure. Not only will you impact on the management on the patient but it is also frustrating at follow up to match the previous measurements
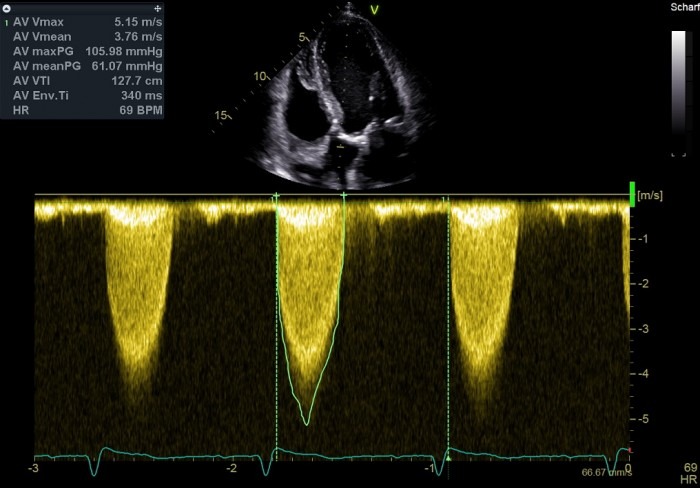
The maximal velocity was measured at 5.1m/s. However, the true peak of the curve is lower (more towards 4 meters).
My tip: Try to increase the quality of the spectrum so that you can really see the contours. Stick to the main (brightest) contour
4) You rely too much on the continuity equation
Do you love numbers and cut off values? They can certainly help, but be critical of these numbers. The aortic valve area often does not match the gradients when you are quantifying aortic stenosis. There are many reasons: wrong measurement of the LVOT, shape of the LVOT, fluctuations of velocities, some even suggest that there is a systematic error.
The LVOT in this patient is not only very small but also difficult to measure. Be cautious when using the continuity equation here
My tip: “Over measure” the LVOT to account for its oval shape, this way the AVA will better match the gradients you measured.
5) You are not interpreting the gradients in the context of other findings
Gradients can change very quickly (even in the same patient). Anything that affects stroke volume can play a role: Anxiety, medications (catecholamies, euphylin), heart rate, or a drop in ejection fraction. To better interpret the gradients look at these cofactors. This is where conditions such a low flow low gradient AS comes into play
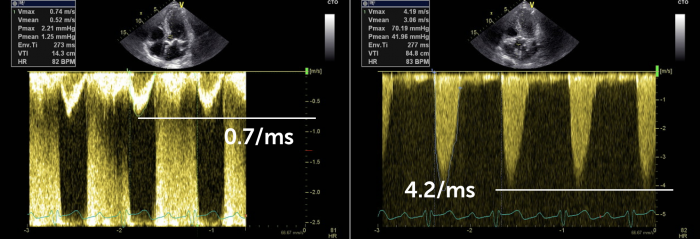
This patient has high gradients across the AV, even though his stroke volume is low (low LVOT velocity). This means the gradients are actually underestimating the true severity. Since the LV can still generate such a gradient there is a good chance that the ventricle will recover after intervention/AV surgery
My tip: Look at the size and function of the left ventricle – but even more so focus on the LVOT velocity, it is an easy surrogate of stroke volume and tells you if the gradients are under- or overestimating the true severity of AS
I hope you enjoyed this part of our teaching series, leave a message, share your views and stay tuned for the next part this series.
Best
Thomas Binder