Cold Feet
In this echo case, we will teach you how to best image the aorta, how to put clinical information into perspective and how to become a true echo expert. Be sure to read the entire piece – we have some goodies for you at the end!
A 70-year-old former bricklayer was sent for echo evaluation directly from the angiology outpatient clinic. Arteries of both legs were occluded – the angiology ultrasound technician suspected an embolic event.
The patient had been anticoagulated for atrial fibrillation only a couple of weeks earlier and was still struggling with his INR – at the time we saw him it was 1.6.
 Parasternal long axis
Parasternal long axis
 Parasternal long axis (Zoom)
Parasternal long axis (Zoom)
Ok, so what do we see…..there is a bit of aortic valve sclerosis. Nothing special. But “oh my god” what the heck was this thing behind the left atrium? Look at the round structure….
We tried to analyze everything systematically:
- Was this the descending aorta?
- Was the moving structure only an artifact?
- Could this finding explain the embolic event?
Well, what we can see behind the left atrium was certainly the descending aorta, which can usually be seen in parasternal-long-axis-views behind the left atrium. To be certain, one can always use color- or PW-Doppler. There, you will find typical systolic flow.
To be sure not to be fooled by an artifact – we used several views and planes. We are sure you all know this? So let us take a look at an apical view and a parasternal short axis view…
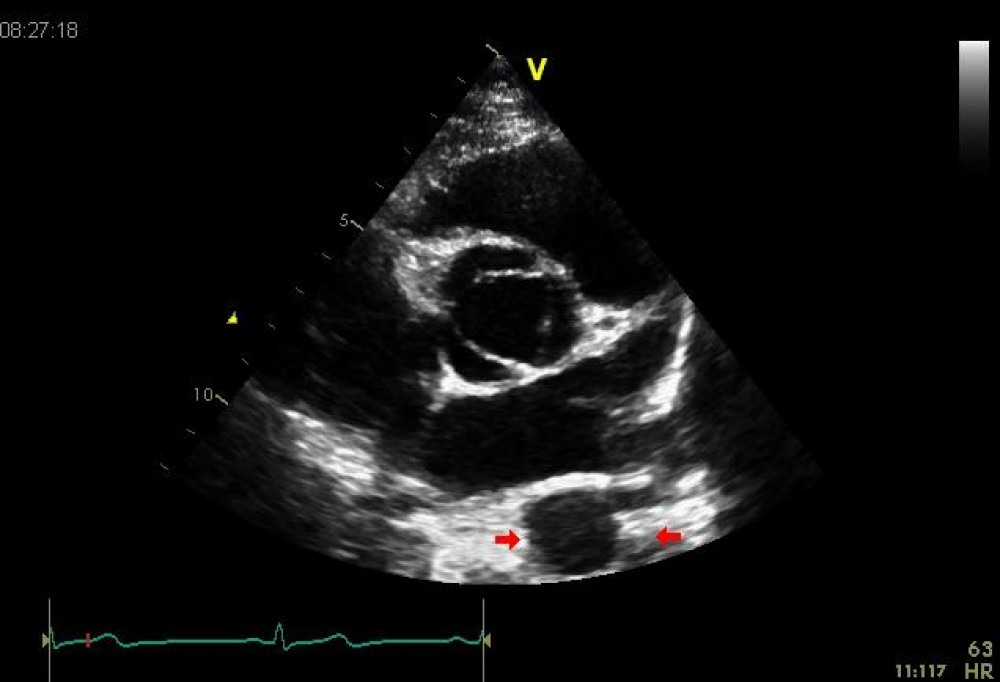
 Apical 4 chamber view
Apical 4 chamber view
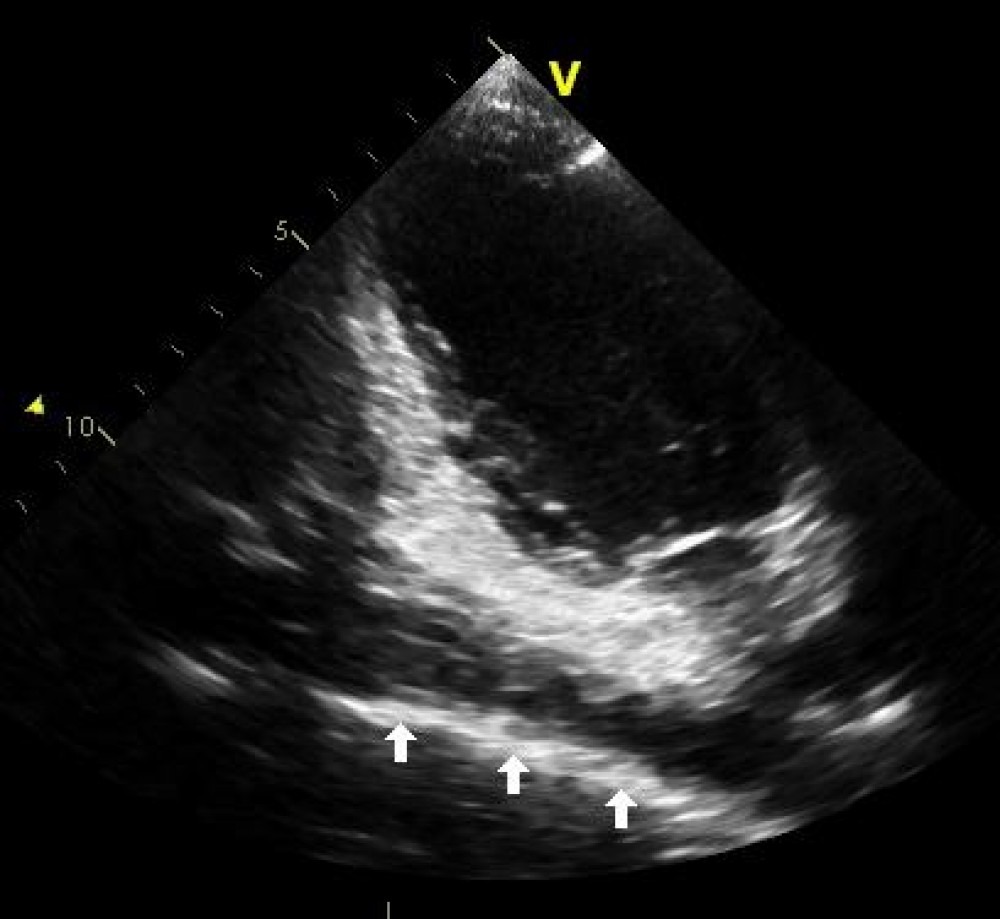
 Parasternal short axis
Parasternal short axis
Rather strange image, right? The right atrium and also the left are dilated. It almost seems as if there was “septation” of the left atrium. Could it be some kind of “cor triatriatum”? But there was no flow between the “upper chamber” and the left atrium. So let us forget that possibility. This must be the descending aorta. Usually the descending aorta can be seen in its long axis in the apical 2-chamber-view, this was not possible in this patient. But we could see it perfectly well in a short-axis-view. The mobile structure could be displayed in all views. So it is a TRUE pathology.
Putting everything together?
We concluded that the patient had kinking and dilatation of the descending aorta (this is why we found it in atypical cut-planes). In addition, we had the suspicion that there was a large plaque with mobile components (a thombus?) in the aorta. Emboli from this plaque are a good explanation for the peripheral embolic events and his cold feet.
Next steps?
We confirmed our findings with a different technique: computed tomography. True, transesophagal echo (TEE) would have also been a possibility, but ultimately CT allowed us to see more of the aorta. All our hypotheses were confirmed. There were massive plaques in the aorta with ulcerations and thrombi. Not only where we found them in the echo but also in the aortic arch and other parts of the descending aorta. From the clinical management point of view – the patient got some additional heparin, until his INR was on the safe side.
What you should remember
Evaluation of the aorta should be a part of every exam. Even though it is mainly the ascending aorta that we can see in echo, there is also a way to visualize the descending aorta.
Here is how it is done: The descending aorta can be visualized in a standard PLAX-view as well as a standard PSAX-view in a cross-sectional view (see images below). If you want to see a longitudinal view, perform an apical 2-chamber view and tilt the transducer left and right. Finally, if the aorta is not displayed in this manner then there is high suspicion that there is kinking of the aorta.
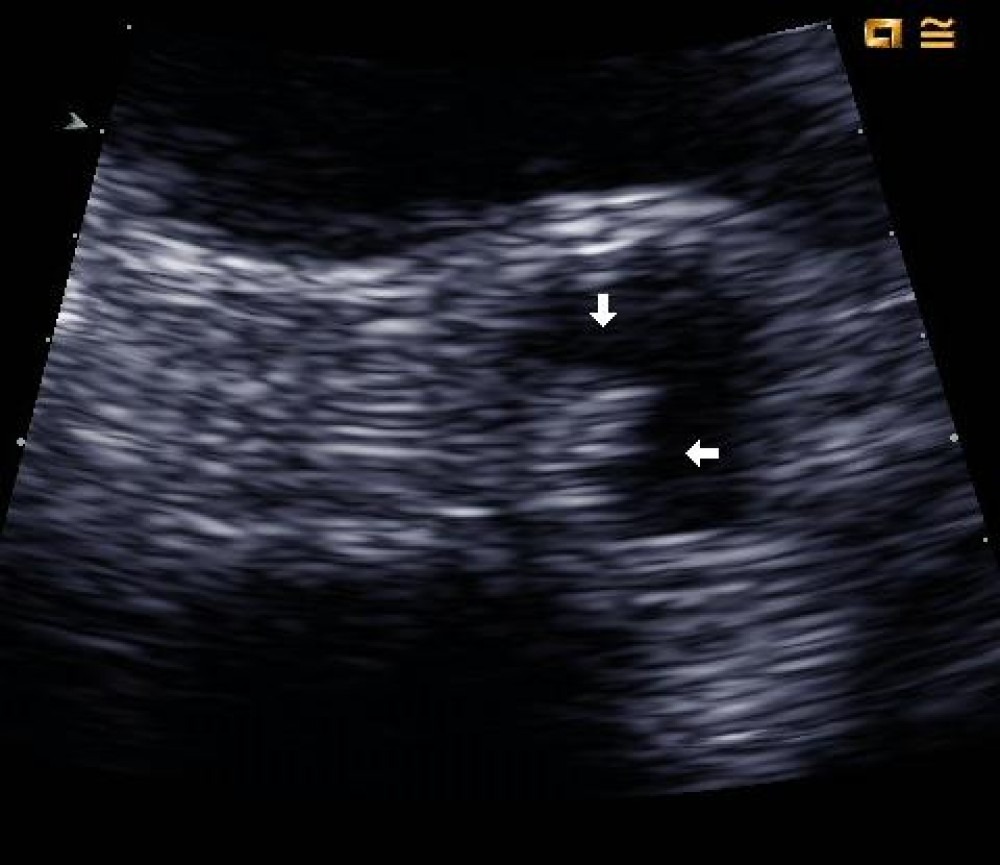
 Short axis - normal individual
Short axis - normal individual
 Atypical 2 chamber view - normal individual
Atypical 2 chamber view - normal individual
You can learn even more about the aorta and how to image it
In our online echo course, we teach you exactly how to visualize the aorta and many other structures. In just 3 months, you will become a true echo expert. If you have not already done so, we encourage you to attend our free chapter on aortic regurgitation right now and immediately advance your echo skills! Just log-in to our classroom with your username and password. Meanwhile, stay tuned for more interesting cases to come.
Recommended articles:
Far From Home
Farmville Echocardiography
Echo Features of a Bicuspid Aortic Valve


