Are you applying the latest guidelines on diastolic function?
Recently I lectured on diastolic dysfunction in India and I asked the auditorium if they were aware of the newest “2016” guidelines on diastolic function and if they were applying them in there patients. I was surprised to find out that while most of the doctors and sonographers in the room knew about them and only 20% applied the guidelines in there patient.
 Lecturing in Bengaluru, India
Lecturing in Bengaluru, India
Why is this so? Are they to complex? Do they have too little time? Interestingly though most of the people in the room still did apply the older 2009 guidelines (65%).
Resistance to change
I believe a main reason is that we are simply resistant to change. The old guidelines were around for 7 years and it took us a while to understand them. Once we did they became routine.
Any type of change into our routine can go against the neural pathways that have become automatic to us. Any new behavior is always counter-balanced by our strive towards homeostasis and working (or having to think) less.
How to read the newest guidelines
What are the key points of the newest guidelines?
In principle the committee emphasizes that in patient with cardiac pathology, where it is clear that diastolic must be present all you need to do is “estimate” the filling pressure to determine the degree of diastolic dysfunction. In all other patients you simply need 4 parameters.
- TDI e ́(lateral and medial)
- TDI E/e
- TR velocity
- Left atrial size
So in reality all you need to do is preselect those patients where you can expect diastolic dysfunction.
Are you ready for a test?
So let us see how easy it is to simply use a four chamber view to “guess if diastolic dysfunction is present. What is your take in these four examples?
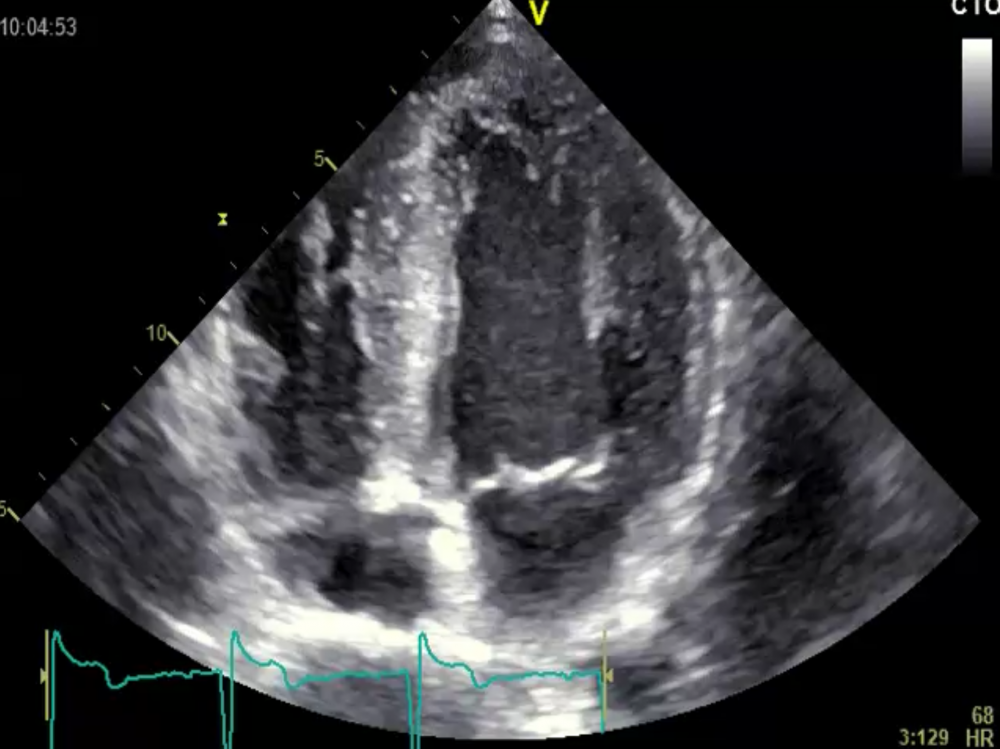 A) A Patient with severe Aortic stenosis
A) A Patient with severe Aortic stenosis
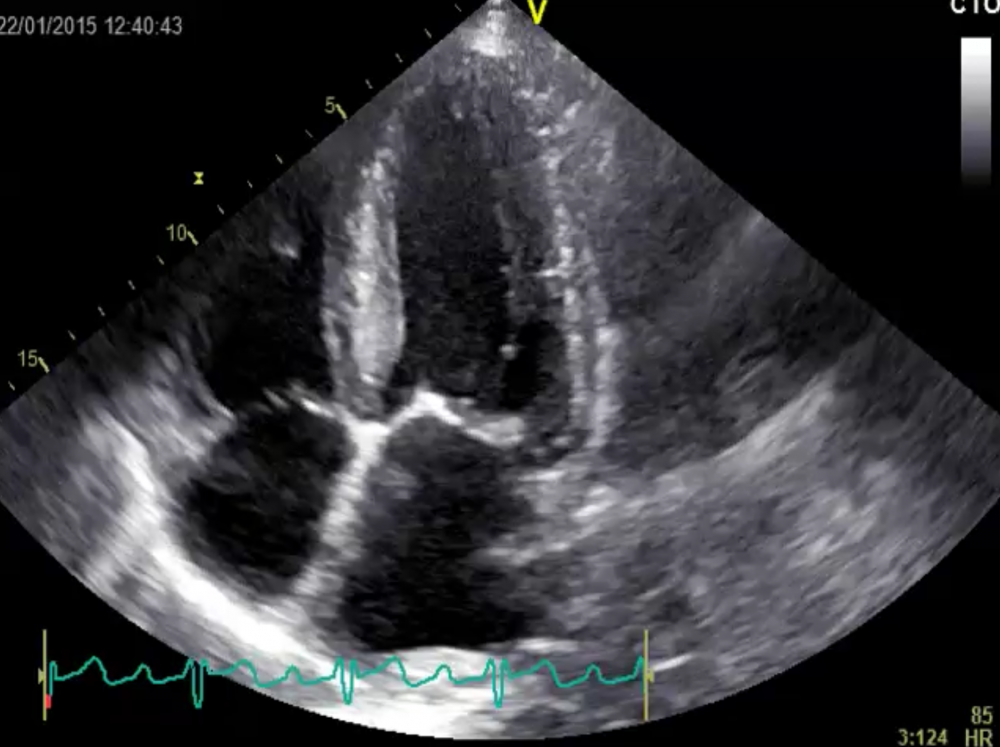 B) A Patient with hypertension and a blood pressure of 210/110mmHg
B) A Patient with hypertension and a blood pressure of 210/110mmHg
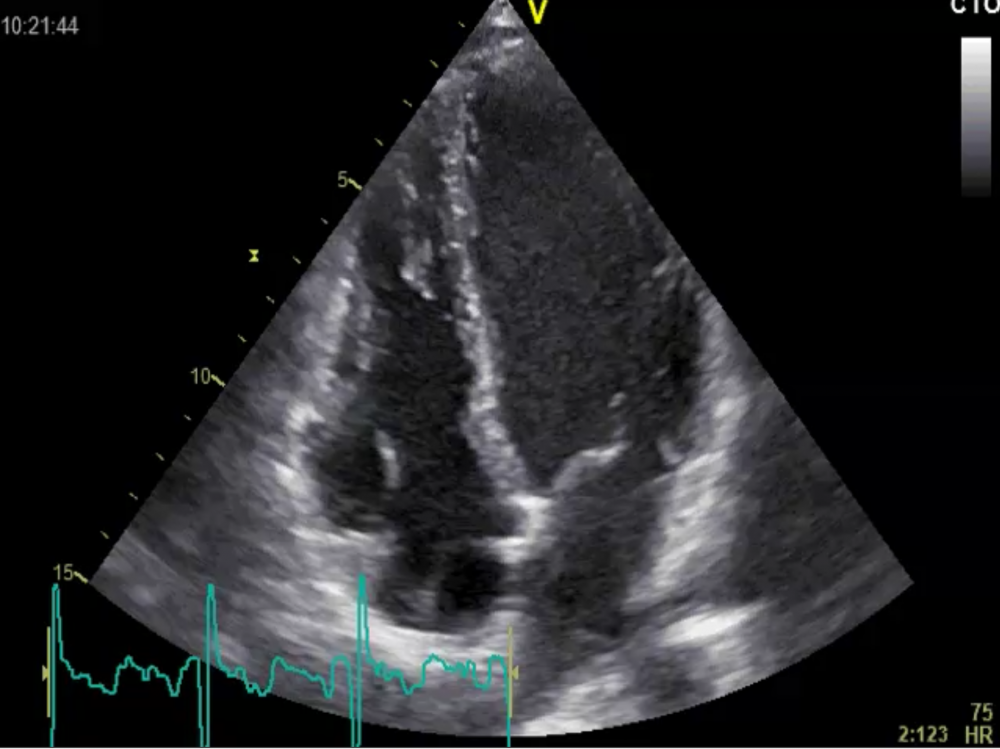 C) A young patient with Preexitation syndrome after successful AV nodal ablation
C) A young patient with Preexitation syndrome after successful AV nodal ablation
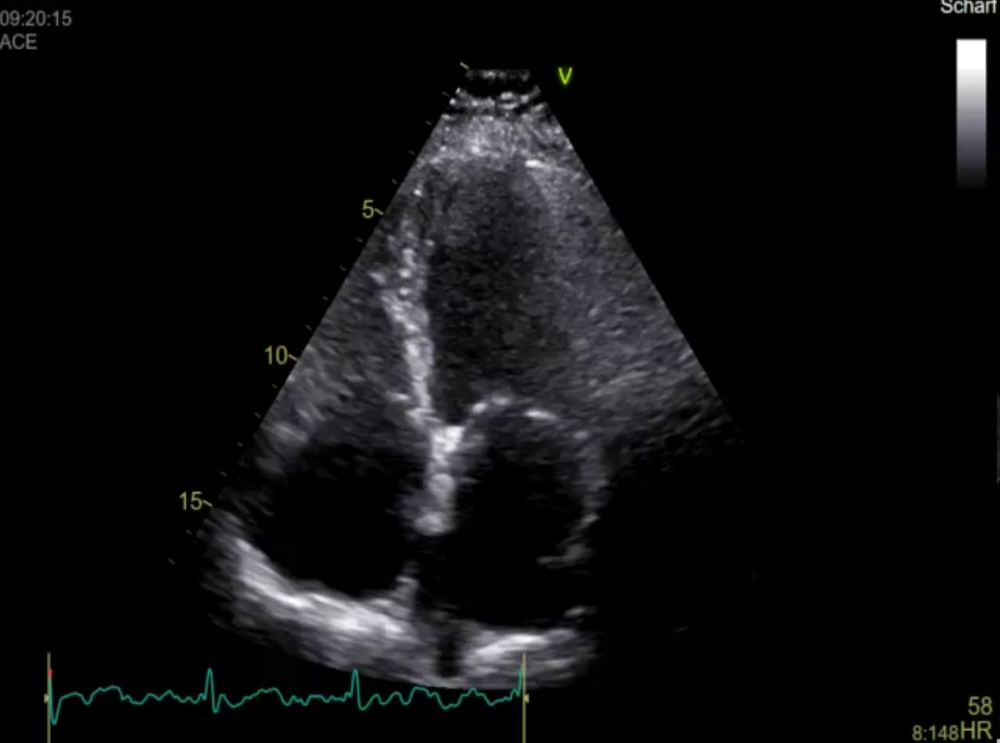 D) An 82 year old diabetic patient with dyspnea
D) An 82 year old diabetic patient with dyspnea
Did you succeed?
I am sure most of you got it right. Clearly, all examples with the exception of the young patient post ablation (C) had diastolic dysfunction. The presence of poor left ventricular function, left ventricular hypertrophy or left atrial enlargement and the presence of dyspnea already suggests the presence diastolic dysfunction.
Lesson learned
What is the lesson learned? Assessing diastolic dysfunction is not “rocket science” and you can get lots of information from the 2D image alone.
Stay tuned for our next newsletter where we will discuss the value of the mitral inflow signal.
Best,
Thomas and the 123sonography team


