2.4 M-Mode
In Chapter 1 we described the basic principles of M-Mode imaging. Here we will discuss how and where one should use the M-Mode. In addition, you will learn about the structures that can be visualized and how the measurements should be performed.
The 2D reference image will help you identify the individual structures you see on the M-Mode.2.4.1 M-mode Parasternal Long Axis of the Aorta
This view is used to measure the width of the aortic root, the separation of the aortic cusps, and the anteroposterior dimension of the left atrium. The M-Mode can be performed from a long or a short axis view. Whichever view you use, make sure that you align the structures perpendicular to the M-Mode. This is done by adjusting the 2D image plane as well as the M-Mode line. It is also important to investigate the aortic root by the M-Mode at the level of the aortic cusps.
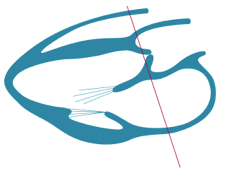 MMode cut plane of the parasternal long axis of the aorta and left atrium
MMode cut plane of the parasternal long axis of the aorta and left atrium

 MMode parasternal long axis of the aorta/left atrium
Optimize your 2D image before you use the M-mode.
MMode parasternal long axis of the aorta/left atrium
Optimize your 2D image before you use the M-mode.
The first reflector that the ultrasound M-mode ray hits (and which is therefore depicted in the near field of the M-mode tracing) is the anterior wall of the right ventricle. To be more specific, you will see the "right ventricular outflow tract" here. Posterior to the right ventricular outflow tract is the anterior wall of the aortic root.
Between the anterior and the posterior wall of the aortic root you will see the aortic valve. Distal to the aortic root is the left atrium.
As you will remember from Chapter 1, the M-mode shows the motion of structures along the time axis. The M-mode tracing will show that the aortic root moves anteriorly during systole and posteriorly during diastole.
The extent of systolic and diastolic excursions of the aortic root reflects ventricular functionWhen the aortic valve opens during systole, the cusps separate. However, on the M-mode image you will only see two cusps. The aortic valve looks like a box. The right coronary cusp is seen in the near field. Which other cusp you see depends on the exact orientation of the M-mode. If the M-mode is more to the left you will see the anterior cusp. If the mode traverses more to the right you will see the acoronary cusp. The cusp may reveal a fine "flutter" motion. This is not a pathologic finding. It is caused by blood flow across the valve, similar to the way the wind "moves" a flag.

 M-mode parasternal long axis of the aorta/left atrium with a fine flutter motion of the aortic valve
M-mode parasternal long axis of the aorta/left atrium with a fine flutter motion of the aortic valve
During diastole, when the aortic valve is closed the M-mode tracing simply shows a line which parallels the motion of the aortic root. The ability to obtain a good M-mode tracing of the aortic valve depends on the quality of the image as well as the echogenicity of the valve.
The size of the left atrium varies during the cardiac cycle. It is largest during end systole. In patients with sinus rhythm you will also note a little "notch" in the motion of the anterior wall of the left atrium (= posterior wall of the aortic root) during late diastole. This notch reflects atrial contraction.
The M-mode tracing across the aortic root and the left atrium serves three purposes: it provides morphologic information (thickening of the aortic valve), functional information (i.e. excursion of the aortic root and opening motion of the aortic valve), and permits measurement of the aortic root and the left atrium. The aortic root is measured at end diastole shortly before the aortic valve opens while the left atrium is measured during end systole (when the aortic valve closes).
M-mode measurements should always be performed along a straight line (you cannot measure distances between structures at different time points).In clinical practice, M-mode measurements of the aortic root and the left atrium may be quite inaccurate because it may be difficult to align the M-mode in perpendicular fashion. Therefore, measurements should not be performed when the mode cannot be aligned properly. More on this subject is given in Chapter 3, which deals with heart chambers and how to measure them.
2.4.2 M-mode at the Level of the Mitral Valve
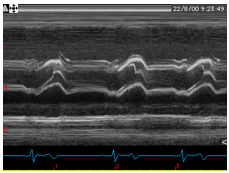
This application of the M-mode was very important in the early days of echocardiography, prior to the discovery of two-dimensional imaging. It displays mitral valve motion and was mainly used to quantify mitral stenosis as well as visualize mitral valve prolapse and systolic anterior motion (SAM) of the mitral valve in hypertrophic cardiomyopathy. Currently this is achieved solely with 2D imaging. The M-mode provides little additional information in the presence of these pathologies. However, it can be used to study the motion of the leaflets (e.g. atrial fibrillation) and detect structures on the mitral valve (e.g. endocarditis). To obtain the M-mode tracing the M-mode line is placed at the tip of the mitral valve from a long- or a short-axis parasternal view. The tracing will show the biphasic opening motion of the mitral valve (when a sinus rhythm is present). The motion of the posterior leaflet is discordant with that of the anterior leaflet.

 M-mode at the level of the mitral valve
M-mode across the mitral valve can be useful to document the "fluttering motion" of the mitral valve in atrial arrhythmia and to assess vegetation.
M-mode at the level of the mitral valve
M-mode across the mitral valve can be useful to document the "fluttering motion" of the mitral valve in atrial arrhythmia and to assess vegetation.
2.4.3 M-mode - Left Ventricle
Probably the most important and widely used application of the M-mode is to measure the dimensions and fractional shortening of the left ventricle. This M-mode tracing can be acquired from a short- or a long-axis view. The M-mode line passes through the basal segment of the left ventricle somewhere between the mitral valve and the papillary muscle. It is very important to ensure that the M-mode line is perpendicular to the walls of the left ventricle. More information on this subject is provided in Chapter 3 under the discussion of measurements.

 MMode at the level of the left ventricle
MMode at the level of the left ventricle
The M-mode tracing reveals the following structures: the free right ventricular wall, the interventricular septum, and the posterior (posterolateral) wall of the left ventricle. Within the left ventricle you will often find chordal structures that execute motions very similar to those of the mitral valve.
The size of the right and the left ventricle and the thickness of the walls of the left ventricle vary during the cardiac cycle. It is simple to depict systole and diastole on the tracing. During diastole you may see biphasic enlargement of the left ventricular cavity, which is a sign of early and late diastolic filling.
2.4.4 Other Applications of the M-mode
The M-mode can be of use in several other settings. These include documentation of the independent flutter motion of a vegetation in a valvular structure, displaying respiratory variations of the inferior vena cava, and differentiating true structures from reverberation artifacts (e.g., when aortic dissection is suspected). In addition, the M-mode can be combined with other echo modalities such as color Doppler or tissue Doppler. The color M-mode permits the investigator to view the propagation of mitral inflow into the left ventricle. This topic will be discussed in greater detail in Chapter 4, which deals with diastolic function.
 Color M-mode showing flow propagation into the left ventricle
Color M-mode showing flow propagation into the left ventricle
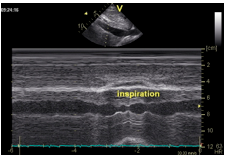 M-mode of the inferior vena cava during inspiration
M-mode of the inferior vena cava during inspiration