12.5 How to assess the mitral valve
Both, standard and apical views will be needed to explore the mechanism of mitral regurgitation and determine the exact location of the pathology. Each of these views shows a different section of the mitral valve. Parasternal and apical views are helpful. On a parasternal short-axis view of the mitral valve you will be able see the "entire" valve and all of its segments, including the commissural regions. The pathology (i.e. prolapse) may be difficult to identify here. The main advantage of this view is its ability to determine the origin of the jet(s) with color Doppler.

Short-axis view in a patient with mitral valve prolapse of the middle scallop of the posterior leaflet (P2). The defect can also be viewed in the 2D image. Short-axis view in a patient with a comissural mitral regurgitation jet.
Coronary sinus view with mitral regurgitation originating from the posterior commissure. If you are an expert in assessing the mitral valve with transthoracic echo, you will need transesophageal studies less frequently.The parasternal long-axis is also helpful. To scan the valve, tilt the transducer parallel to the long axis. Tilting the transducer "downward" will demonstrate the posteromedial segments while tilting upward will show the anterolateral segments.
Apical views also permit thorough assessment of the valve. This is best done by starting with a four-chamber view - with the mitral valve in the middle of the sector - and then rotating the transducer around the axis of the mitral valve. The following figure shows the exact orientation of the apical standard views through the mitral valve.
In general, when assessing the mitral valve for regurgitation it is better to use a "sweep" technique rather than to stick to standard views.
How to visualize MV segments
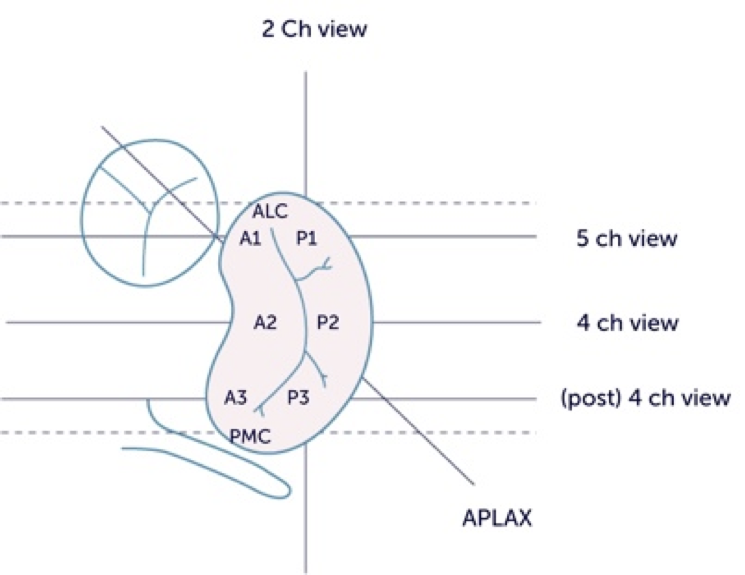
On a four-chamber view you will see the middle scallops of the anterior and posterior leaflet. By tilting the transducer towards a five-chamber view, the anterolateral segments (A1 and P1) and the anterolateral commissure will become visible. When tilting towards the coronary sinus view A3, P3 and the postero-medial commissure are seen. Again, use 2D imaging and color Doppler to identify the location and extent of the defect. On the apical long-axis (three-chamber) view, the posterior leaflet is cut somewhere between P2 and P3 while the anterior leaflet is at A1.
On the two-chamber view it is not possible to differentiate between the anterior and the posterior leaflet because you are parallel to the line of closure. However, this view is ideal to determine whether the pathology is located in the anterolateral (1), the middle (2), or the posterolateral (3) portion of the valve. Both commissures are also seen. In clinical practice you may need to modify the two-chamber view in order to display a true "commissural view".
Very frequently more than one jet will be present.