5.4.5.Diastolic dysfunction and filling pressures
Diastolic dysfunction exists in all patients with dilated cardiomyopathy. As systolic dysfunction is always associated with diastolic dysfunction, the assessment of diastolic function and filling pressures is very important in patients with dilated cardiomyopathy. It provides valuable information concerning the severity of the disease and its prognosis. Filling pressures correlate well with the symptoms and magnitude of pulmonary hypertension. Diastolic function may be assessed using the mitral inflow signal, tissue Doppler at the mitral annulus, and all other modalities described in Chapter 4. However, caution is advised when using the E/e´ratio, because it is unreliable in the setting of reduced left ventricular function (link). Diastolic dysfunction cannot be assessed in the presence of moderate to severe mitral regurgitation
Assessment of diastolic function is very valuable in patients whose pulmonary pressure cannot be measured, because diastolic function correlates well with the symptoms and prognosis of the condition. Video Platform Video Management Video Solutions Video Player Diastolic function correlates with symptoms. Both of the patients shown above have dilated cardiomyopathy and severely reduced left ventricular function. However, the patient with a restrictive filling pattern (right) suffers from class III-IV heart failure, whereas the patient with impaired relaxation (left) has class I-II disease5.4.6 Left atrial enlargement
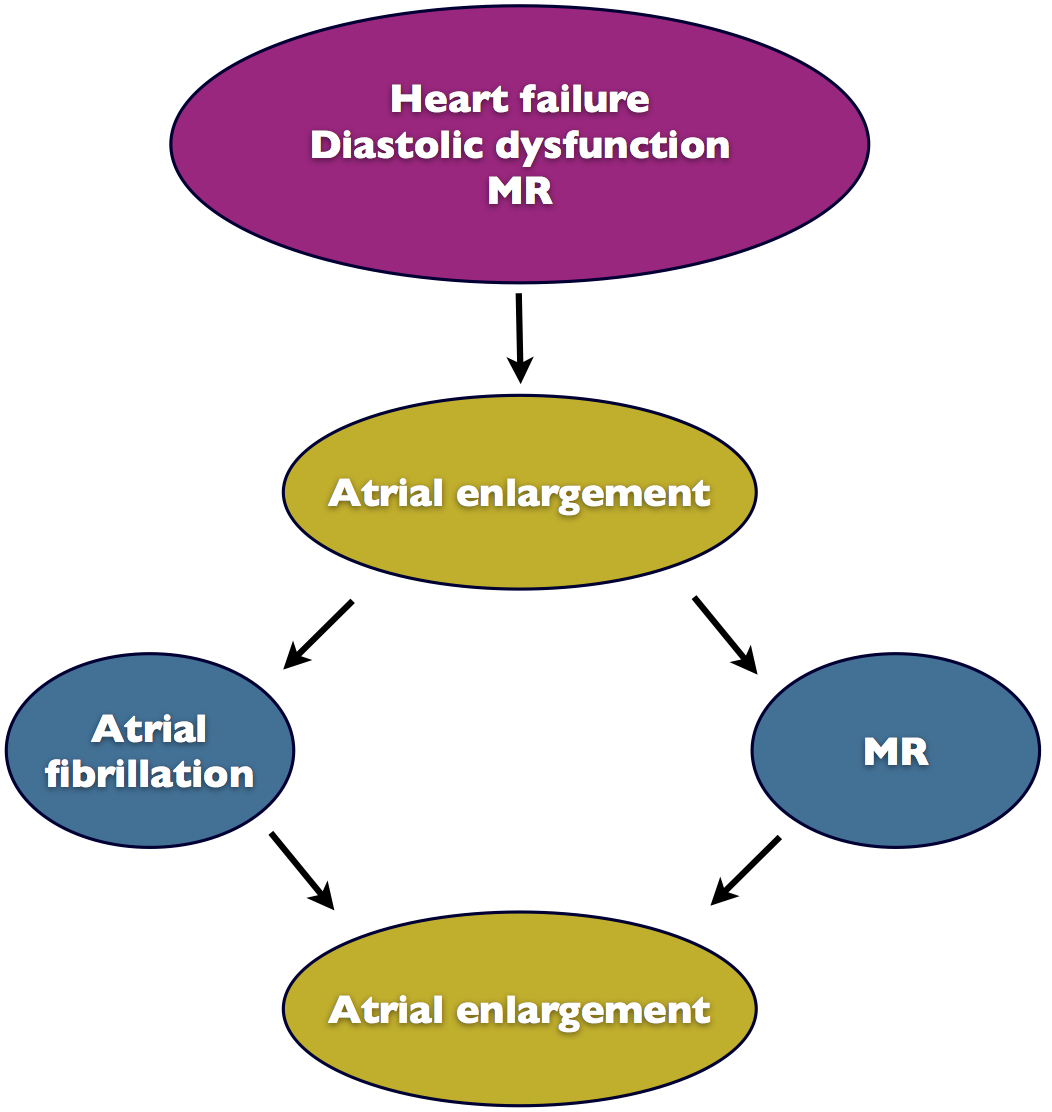
Left atrial enlargement is the result of elevated filling pressures (diastolic dysfunction), mitral regurgitation, and atrial fibrillation. The size of the atrium is correlated with the severity and duration of the disease. Thus, atrial size may be used as an additional parameter to study patients with dilated cardiomyopathy.
Volume measurements should be given preference over distance and area measurements. The measurements should ideally be indexed to the body surface area.
Atrial enlargement is associated with an adverse prognosis. The larger the atrium, the higher is the risk of hospitalization, mortality, atrial fibrillation, and stroke. When the left atrial volume index is more than 68.5 ml/m2, the risk ratio of a major event is 3.8.
Video Platform Video Management Video Solutions Video Player A patient with a rather small left atrium despite poor left ventricular function and a very large ventricle. Note that the right ventricle is also small and its function is normal. This patient has just mild symptoms.There is evidence of the fact that atrial enlargement also contributes to annular dilatation. Thus, atrial enlargement might play a role in the development of functional mitral regurgitation, which is common in patients with dilated cardiomyopathy.
In summary, dilatation of the left atrium triggers a vicious circle because it predisposes the individual to atrial fibrillation and fibrosis of the atrial wall, which in turn causes further enlargement of the atrium.
5.4.7 Functional mitral regurgitation
Functional mitral regurgitation is a common finding in patients with dilated cardiomyopathy. Mitral valve incompetence is caused by two major mechanisms: annular dilatation and leaflet restriction. Annular dilatation is the result of dilatation of the ventricle at the base. The leaflets are dragged apart, leaving a "central" coaptation defect (see Chapter 12 Mitral Regurgitation). Leaflet restriction is the result of global ventricular dilatation which alters ventricular geometry. Papillary muscles are displaced and the chordae exert tension on the mitral valve leaflets. The leaflets are pulled towards the apex and positioned more laterally. Motion of the leaflets is restricted, preventing closure of the valve. Depending on the geometry of the ventricle, leaflet restriction may affect one or both leaflets.
Look at the plane of closure of the mitral valve. In restricted leaflets it is further within the ventricle than in annular dilatation.The combination of restriction and annular dilatation is very common. Patients with leaflet restriction react very "sensitively" to annular dilatation. A mild degree of annular dilatation will result in a large increase in mitral regurgitation in these patients.
Video Platform Video Management Video Solutions Video Player Functional mitral regurgitation (restriction and annular dilatation) in dilated cardiomyopathy. The jet is oriented centrally and is very large.This is also the reason why the degree of mitral regurgitation may vary in these patients. Regurgitation may be severe one day and mild a few days (or even hours) later. Mitral regurgitation showing significant variations in severity is also referred to as "dynamic" mitral regurgitation. Factors that affect pre- and afterload of the ventricle and, consequently, left ventricular size, may greatly influence the degree of mitral regurgitation. Decompensation, fluid overload, hypertension, exercise, or tachycardia may increase in mitral regurgitation, which is completely reversible.
Stress echocardiography can be helpful in detecting dynamic mitral regurgitation. Dynamic mitral regurgitation is common in patients with dilated cardiomyopathy.The degree of mitral regurgitation not only depends on the size of the ventricle but also on its geometry and regional function. Although patients with large ventricles are more likely to have severe mitral regurgitation, this is not true of all patients. The contractile function of the mid-lateral wall also plays a role. Besides, individual anatomic characteristics of the mitral valve could either predispose an individual for, or protect him/her against, valvular incompetence.
In the presence of mitral regurgitation, left ventricular function appears better than it is.Patients with dilated cardiomyopathy and mitral regurgitation have a poor prognosis. Not only does volume overload pose an additional burden to the ventricle, but mitral regurgitation itself aggravates mitral regurgitation (via further annular dilatation).
Mitral valve repair is no option for patients with severely reduced left ventricular function. Percutaneous mitral valve repair techniques (e.g. MitraClip procedure) are promising new treatment options for patients with reduced left ventricular function and severe mitral regurgitation.When assessing patients with reduced left ventricular function and mitral regurgitation, make sure not to miss a structural form of mitral regurgitation. In this case the cause of cardiomyopathy might be "valvular" as opposed to dilated cardiomyopathy. In other words, mitral regurgitation is the cause and not the consequence of reduced left ventricular function. It is important to distinguish between the two forms of cardiomyopathy because they require different treatment strategies. The direction of the jet may be helpful to distinguish between the two types. The jet is rather centrally oriented in patients with functional mitral regurgitation, whereas it is more eccentric in those with primary causes (flail leaflet or mitral valve prolapse).
Look for diastolic mitral regurgitation. It may be present in the setting of elevated filling pressure, dyssynchrony, or prolonged AV conduction.5.4.8 Right ventricular dysfunction
Many patients with dilated cardiomyopathy have right ventricular dysfunction. It may be the result of right ventricular myocardial involvement or post-capillary pulmonary hypertension secondary to left ventricular dysfunction. Right ventricular function is closely linked to the prognosis and symptoms. Patients may be relatively asymptomatic despite severely reduced left ventricular function as long as right ventricular function is preserved. But once right ventricular function deteriorates, the patient will develop symptoms - especially those of right heart failure (peripheral edema, pleural effusion, etc.).
5.4.9 Pulmonary hypertension
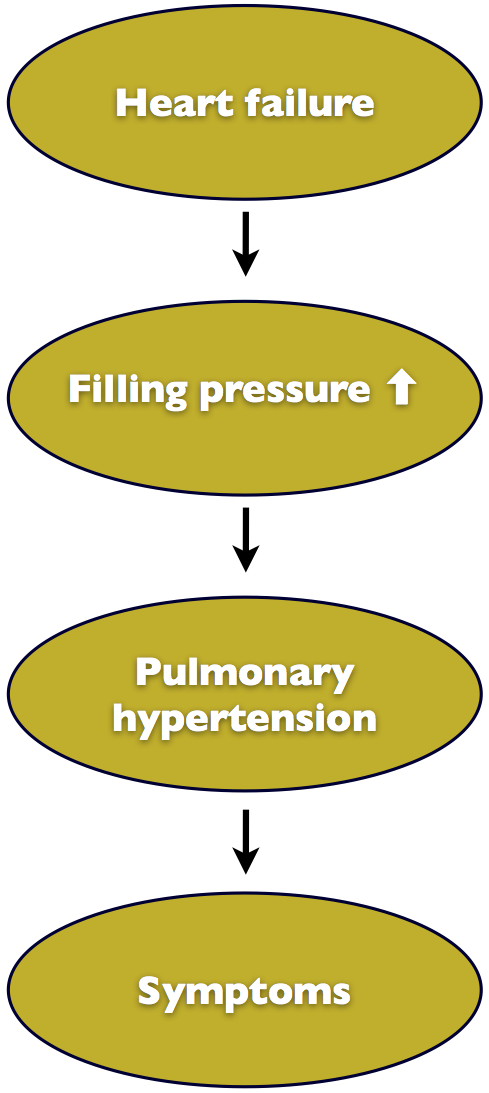
Pulmonary hypertension is a very powerful predictor of death and the need for heart transplantation in patients with cardiomyopathy. In patients with reduced left ventricular function, pulmonary hypertension is the result of elevated filling pressures that translates to the pulmonary veins and eventually causes post-capillary pulmonary hypertension. Mitral regurgitation, which is frequently present in patients with left heart failure, also contributes to pulmonary hypertension. Post-capillary pulmonary hypertension may also be associated with a reactive increase in pulmonary vascular resistance that is superimposed on pulmonary venous pressure.
Pulmonary pressure correlates well with the symptoms of dyspnea. This is not surprising because post-capillary pressure causes alveolar edema and therefore dyspnea. Furthermore, pulmonary hypertension affects right heart function. It may eventually lead to right heart failure and significant tricuspid regurgitation. Pulmonary pressure is a useful parameter to monitor therapy because it also drops when the patient receives treatment that reduces filling pressure (e.g. diuretics, heart failure therapy).
5.4.10 Tricuspid regurgitation
Moderate or severe forms of tricuspid regurgitation are frequently seen in patients with dilated cardiomyopathy. Right ventricular dysfunction and right ventricular dilatation predispose an individual to tricuspid annular dilatation and therefore tricuspid regurgitation.
The presence of tricuspid regurgitation is also associated with a poor prognosis; it predisposes the individual to right ventricular dysfunction.
5.4.11 Intracardiac thrombi
Patients with impaired systolic function are at high risk of developing left ventricular as well as left atrial thrombi. The incidence of thromboembolism in such patients is between 1.5 to 3.5/100 patient-years. Patents with very poor left ventricular function, very large ventricles, large left atria, and spontaneous echo contrast, are subject to a particularly high risk of thrombi. The risk is even greater when atrial fibrillation develops. In contrast, mitral regurgitation reduces the risk of left ventricular thrombus formation because volume overload also increases blood flow velocities and irrigates of the ventricle.
Video Platform Video Management Video Solutions Video Player Atypical view of a patient with severely reduced left and right ventricular function. A thrombus is seen in the right ventricular apex. Severe mitral regurgitation possibly exerts a protective effect as regards ventricular and atrial thrombi.Thrombi may also be present in the right heart, especially when right ventricular function is reduced. Echocardiography is able to detect thrombi in all chambers of the heart. However, in most cases left thrombi confined to the left atrial appendage cannot be seen with transthoracic echocardiography. A transesophageal echocardiography must be performed in these patients.
Search for a thrombus in every patient with dilated cardiomyopathy.5.5 General remarks
Dilated cardiomyopathy is characterized by ventricular dilatation and impaired function. By definition, all patients with dilated cardiomyopathy share these features. However, each case of dilated cardiomyopathy has its characteristic footprint, which is defined by several other factors: the exact shape of the ventricle, the degree of left ventricular function, size and function of the right ventricle, the presence of dyssynchrony, the degree of valvular incompetence, and many others. It is these differences that determine symptoms, prognosis, and the best therapeutic approach. With echocardiography it is possible to investigate all of these factors. Ultimately, the ability to "see" even subtle differences is a crucial aspect of truly understanding the problem. This knowledge, and a profound knowledge of the disease, will ultimately translate into better management of patients.
