13. Vertebral Artery Pathologies
/* .lity-iframe-container iframe { background: #fff !important; } */ .articles__categories nav { display: none !important; } .sonopl-book__aside .articles__categories { background: #f5f5f5; } .sonopl-article th, .sonopl-article td { color: black; text-align: left; } function advagg_mod_1() { // Count how many times this function is called. advagg_mod_1.count = ++advagg_mod_1.count || 1; try { if (advagg_mod_1.count <= 40) { var getClass = document.querySelectorAll(".articles__categories"); var a = document.createElement('a'); var linkText = document.createTextNode("Get Carotid MC Free Lectures"); a.appendChild(linkText); a.title = "newsletter"; a.href = "/overlay/forms/cu_mc/16618"; a.setAttribute("class", "sonopl-button sonopl-button--default"); a.setAttribute("data-lity", ""); a.style = "line-height: 1.2;margin-top: 25px;padding: 15px;width: 100%;"; for(var ix = 0; ix < getClass.length; ix++) { getClass[ix].appendChild(a) } // Set this to 100 so that this function only runs once. advagg_mod_1.count = 100; } } catch(e) { if (advagg_mod_1.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_1, 250); } } } function advagg_mod_1_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_1(); } else { window.setTimeout(advagg_mod_1_check, 250); } } advagg_mod_1_check();
13.1 Why should you perform ultrasound of the vertebral arteries?
The vertebral arteries contribute 15-25% of the blood supply to the brain (100-200ml). This is significantly less than the carotid arteries. Still, the vertebral arteries (and the vertebro-basilary system) play and important role in the cerebro-vascular circulation. The vertebral arteries supply the:
- Posterior part of the brain
- Brain stem
- Cerebellum
- Upper spinal chord
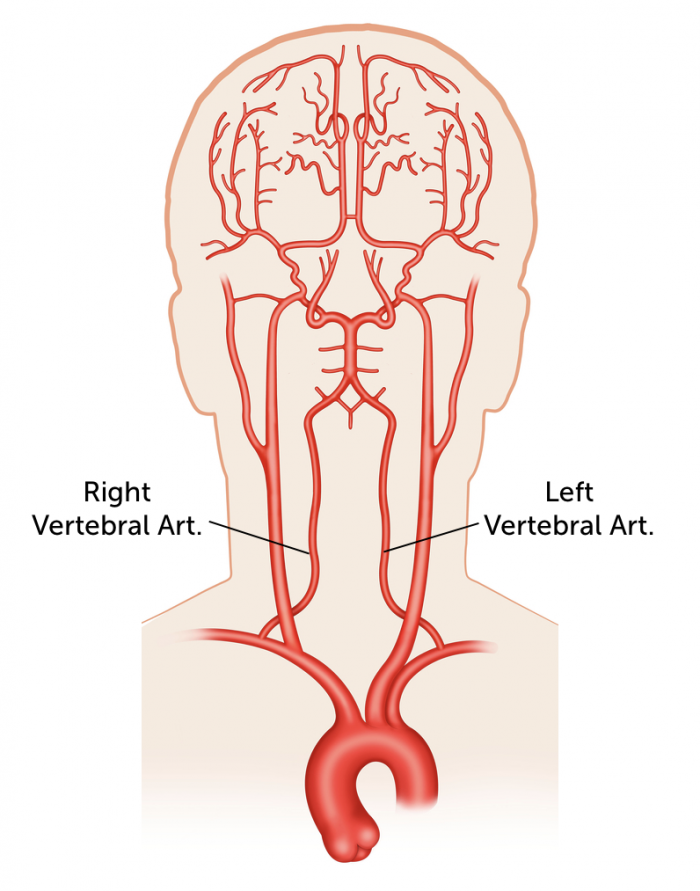 VA Blood supply: blood supply of the brain. The vertebral artery supplies the 15-25% of the brain
VA Blood supply: blood supply of the brain. The vertebral artery supplies the 15-25% of the brain
In addition, the vertebral arteries can provide collateral blood flow in the presence of an innominate – or proximal subclavian artery occlusion (subclavian steal syndrome) as well as in occlusion of the common / internal carotid arteries.
It is mandatory to also examine the vertebral arteries during a full carotid ultrasound duplex study especially, if there is clinical evidence for ischemia of the posterior circulation (i.e. dizziness, nausea, vertigo, dysarthria, loss of balance). Aside from obstructive atherosclerotic lesions you might also find hypoplasia/aplasia or dissection of the vertebral arteries.
13.2 Why is it more difficult to image the vertebral arteries?
Imaging of the vertebral arteries can sometimes be technically challenging as the vertebral arteries are smaller, lie further in the far field and the vertebral arteries are partially hidden behind the bony structures of the transverse processes. With experience and the correct technique it is possible to visualize and identify the vertebral artery in the vast majority of patients (find more on how to image the vertebral artery see Chapter 7)
Note: The segment V2 can be seen in 98% of patients, the origin (segment V1) of the right vertebral artery in 92-94%. The origin of the left vertebral artery is most difficult to image (60-86%).
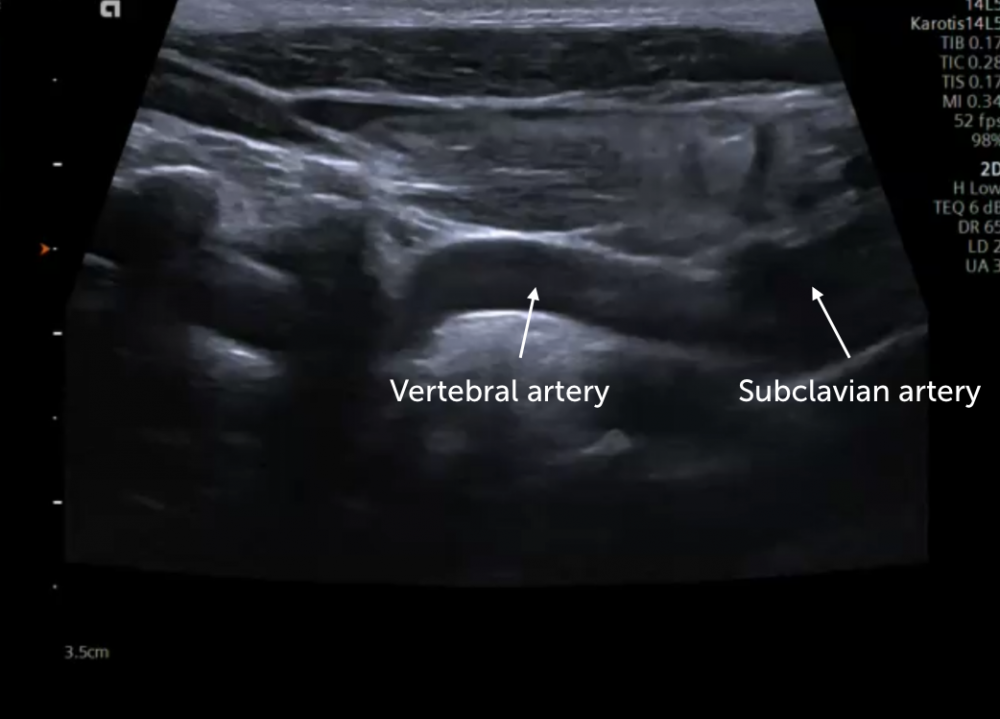 Normal Vertebralis scan: ultrasound scan of the vertebral artery in a young healthy individual.
Normal Vertebralis scan: ultrasound scan of the vertebral artery in a young healthy individual.
13.3 What should you look for when imaging the vertebral arteries?
It is important to perform both B-Mode imaging, Color Doppler and Spectral Doppler of both vertebral arteries. The following features should be assessed:
What to look for when imaging the vertebral arteries
B Mode Color Doppler Spectral Doppler Size Flow direction Wave form Plaque stenosis Turbulance Max velocity Dissection / Thrombus
13.4 What is a hypoplastic vertebral artery
It is quite common to find dominance of one vertebral vessel (usually the left vertebral artery). Hypoplasia can be seen as an extreme form of a size discrepency between the two vertebral arteries. Hypoplasia of the vertebral artery is a congenital defect (incidence: 2-6%) defined by a diameter: < 2-3 mm (ratio >1:1.7). Patients with hypoplastic vertebral arteries are usually asymptomatic and the pathology is frequently discovered incidentally during ultrasound, MRI or CT-Angiography.
Note: It is advised to routinely measure the size of the vertebral arteries with ultrasound
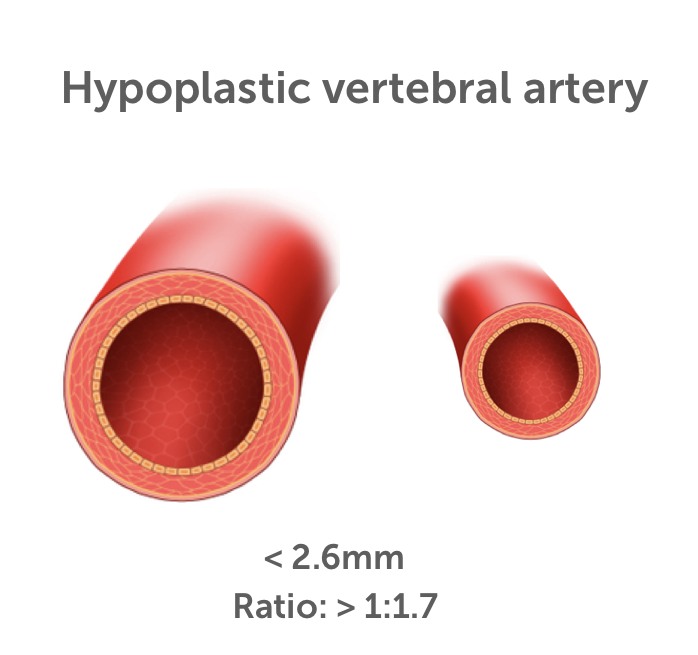 Hypoplastic VA Definition of hypoplastic vertebral artery
Hypoplastic VA Definition of hypoplastic vertebral artery
Note: The flow velocity in a hypoplastic artery is less than that in the contra-lateral vertebral artery.
The clinical relevance of hypoplasia of the vertebral artery is unclear: There are reports of an association between hypolastic vertebral arteries and migraine and studies have shown that pontine infarcts are twice as common in such patients. Hypoplasia can also result in lack of compensation in stroke.
13.5 What if I don’t find the vertebral artery?
There are three possibilities:
- You missed it: Check carefully also using color Doppler and consider that it may be hypoplastic and therefore more difficult to find.
- It is occluded: Check at the origin, this is where occlusions are most commonly located
- It is absent (agenesis of the carotid artery)
A large contra-lateral vertebral artery often points to a hypoplastic vertebral artery or to agenesis of the vertebral artery.
Other imaging modalities (CT or MRI-Angiography) are often required to confirm or exclude the presence of occlusion or agenesis of the vertebral artery.
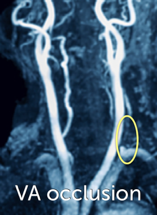 MRI VA. MRI-Angiogram demonstrating occlusion of the vertebral artery
MRI VA. MRI-Angiogram demonstrating occlusion of the vertebral artery
13.6 How can I detect a stenosis or occlusion of the vertebral artery?
A stenosis or occlusion of the vertebral artery is most commonly found at the origin of the vertebral artery. Some degree of stenosis can be found in the vertebral artery (more commonly in the left vertebral artery) in approximately 18-23% of patients with an ischemic stroke. The vertebral artery is the second most common site of ischemic stroke following the proximal carotid artery.
Typical findings of vertebral artery stenosis / occlusion include: Narrowing of the artery / plaque, flow acceleration, occluded vessel (no flow detectable with color- and spectral Doppler)
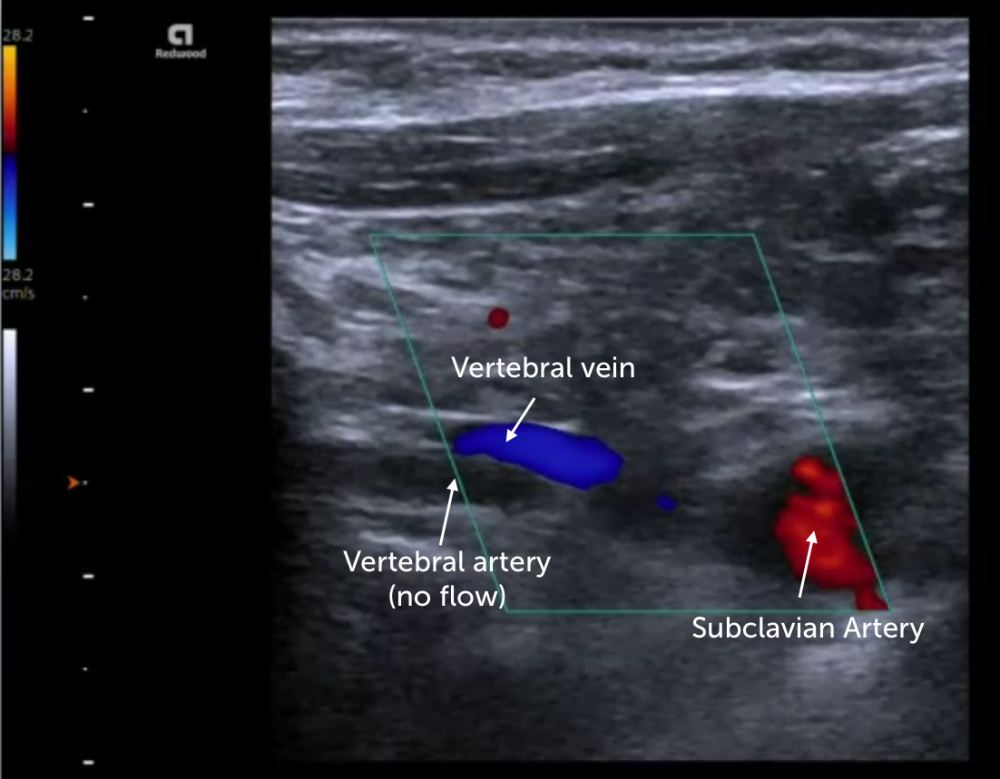 Vertebral artery occlusion: typical finding of vertebral artery occlusion: Absence of color flow within the vessel distal to its origin.
Vertebral artery occlusion: typical finding of vertebral artery occlusion: Absence of color flow within the vessel distal to its origin.
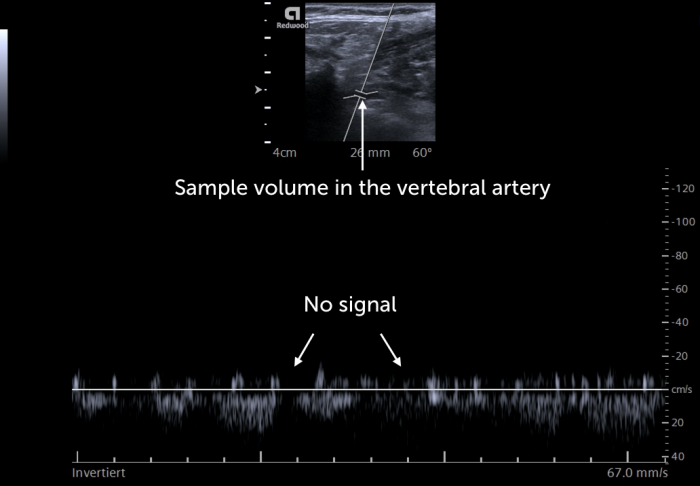 A PW Doppler occlusion: typical findings of vertebral artery occlusion: Absence of a spectral Doppler signal within the vessel distal to its origin
A PW Doppler occlusion: typical findings of vertebral artery occlusion: Absence of a spectral Doppler signal within the vessel distal to its origin
The following table displays the typical ultrasound criteria for vertebral artery stenosis / occlusion:
US criteria
- Focal elevated blood flow velocity (color Doppler)
- PSV ≥ 140cm/s at V1
- PSV ≥ 125cm/s at V2
- Slow systolic rise distal to the stenosis
- High velocity ratio maximal stenotic flow velocity / pre-stenotic velocity (>4 = severe)
- Note: It is often difficult to directly visualize the plaque stenosis (use Doppler!)
Note: You will frequently need to confirm your findings with other imaging modalities (CT, DSA or MRI-Angiography)
Note: Vertebral artery occlusions / stenosis can be treated!
13.7 What is the normal flow velocity in the vertebral artery?
The normal flow velocity in the vertebral artery can vary considerably depending on the size of the vessel (higher flow in dominant vertebral arteries). Normal velocities are between 20-60cm/s.
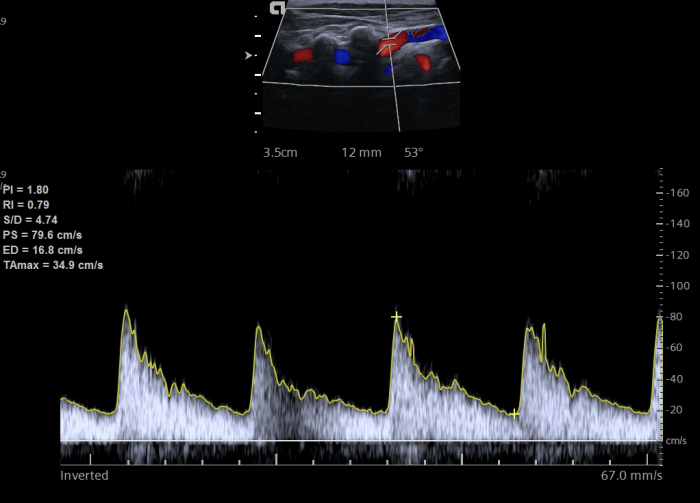 Normal flow VA: Normal, but relative high flow velocity (80cm/s) in the mid vertebral artery in a young individual without any pathologies
Normal flow VA: Normal, but relative high flow velocity (80cm/s) in the mid vertebral artery in a young individual without any pathologies
13.8 What is a dissection of the vertebral artery?
Dissection of the vertebral artery is caused by a tear in the intima/media of the vertebral artery. While vertebral artery dissection is a rare condition (incidence: 1-1.5 per 100.000) it is a common cause of stroke in young individuals. (18-45). Patients with connective tissue disorders (i.e. Marfan syndrome, Ehlers Danlos Disease) are at increased risk for dissection.
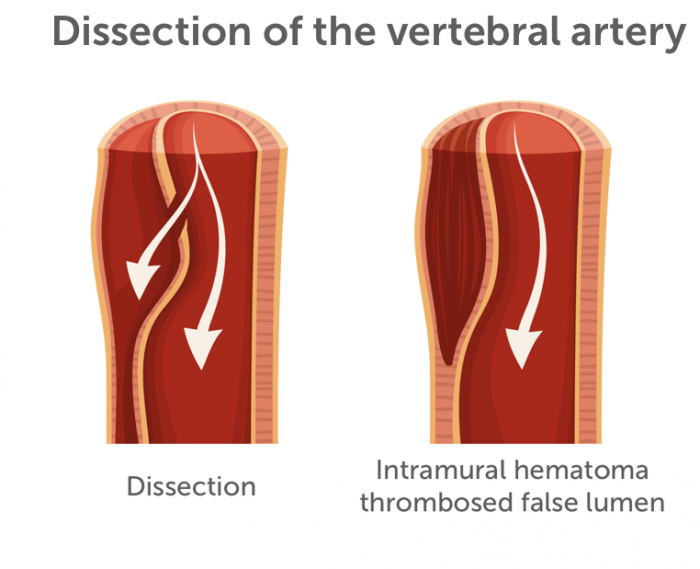 Dissection VA. Principle of dissection (vertebral artery). A tear of the intima separates the intima from the media forming a second lumen. Intramural hematoma/thrombus formation lead to narrowing of the artery and potentially occlusion
Dissection VA. Principle of dissection (vertebral artery). A tear of the intima separates the intima from the media forming a second lumen. Intramural hematoma/thrombus formation lead to narrowing of the artery and potentially occlusion
Dissection can occur spontaneous, following rapid neck movements or after blunt trauma (i.e. traffic accident, strangulation). A dissection is most frequently found in the segments (V2 and V3). Dissection can extend to the intracranial portions of the vertebral artery and cause subarachnoid hemorrhage. Most frequently however, it results in stenosis and occlusion (thrombus, intramural hematoma) of the vertebral artery followed by stroke.
13.9 What will I find with ultrasound in vertebral artery dissection?
Ultrasound features of vertebral artery dissection include:
- Intima flap (dissection membrane)
- Visualization of a false and a true lumen
- Intramural hematoma
- Aneurysms
- Flow impairment / vessel occlusion
- Other imaging modalities (i.e. MRI-angiography, CT Angiography) are usually required to fully assess the pathology and to determine the extent of dissection.
Note: patients with dissection in one extracranial artery are more likely to have a dissection also in other vessels.
.pagination .pager .pager__item { font-size: 12px; } .pagination .pager .pager__item--current { padding: initial; } .pagination { margin: 0; margin: 0 auto; margin-top: 0 !important; } .pager { margin-top: 0 !important; padding: 0; display: flex; } .pagination .pager { padding: 0; } .pagination .pager a { padding: 8px 12px; } .pager__item a { box-shadow: none !important; } .aut-nav-carotid-p { text-align: center !important; margin-bottom: 6px !important; } function advagg_mod_2() { // Count how many times this function is called. advagg_mod_2.count = ++advagg_mod_2.count || 1; try { if (advagg_mod_2.count <= 40) { var autNaviCarotid1 = ('\ \- \
- \
Chapters\
\
- \ 1\ \
- \ 2\ \
- \ 3\ \
- \ 4\ \
- \ 5\ \
- \ 6\ \
- \ 7\ \
- \ 8\ \
- \ 9\ \
- \ 10\ \
- \ 11\ \
- \ 12\ \
- \ 13\ \
- \ 14\ \
- \ 15\ \
- \ last »\ \ \ \ '); var autNaviCarotid2 = ('\
Carotid Ultrasound Webbook & Wiki\ \
- \
- \
‹ previous\
\
- \ BACK TO OVERVIEW\ \
- \ next ›\ \ \ \ '); (function($) { $(document).ready(function(){ $(".sonopl-article.sonopl-book__content.sonopl-content-main") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); $(".aut-nav-carotid") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); }); }(jQuery)); // Set this to 100 so that this function only runs once. advagg_mod_2.count = 100; } } catch(e) { if (advagg_mod_2.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_2, 250); } } } function advagg_mod_2_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_2(); } else { window.setTimeout(advagg_mod_2_check, 250); } } advagg_mod_2_check();
If you like the way we teach, please leave a message!
- \ BACK TO OVERVIEW\ \
- \ 1\ \


