12. Carotid Artery Stenosis Part 2: Spectral Doppler
/* .lity-iframe-container iframe { background: #fff !important; } */ .articles__categories nav { display: none !important; } .sonopl-book__aside .articles__categories { background: #f5f5f5; } .sonopl-article th, .sonopl-article td { color: black; text-align: left; } function advagg_mod_1() { // Count how many times this function is called. advagg_mod_1.count = ++advagg_mod_1.count || 1; try { if (advagg_mod_1.count <= 40) { var getClass = document.querySelectorAll(".articles__categories"); var a = document.createElement('a'); var linkText = document.createTextNode("Get Carotid MC Free Lectures"); a.appendChild(linkText); a.title = "newsletter"; a.href = "/overlay/forms/cu_mc/16618"; a.setAttribute("class", "sonopl-button sonopl-button--default"); a.setAttribute("data-lity", ""); a.style = "line-height: 1.2;margin-top: 25px;padding: 15px;width: 100%;"; for(var ix = 0; ix < getClass.length; ix++) { getClass[ix].appendChild(a) } // Set this to 100 so that this function only runs once. advagg_mod_1.count = 100; } } catch(e) { if (advagg_mod_1.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_1, 250); } } } function advagg_mod_1_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_1(); } else { window.setTimeout(advagg_mod_1_check, 250); } } advagg_mod_1_check();
12.1 How to use Spectral Doppler in the assessment of carotid artery stenosis
Spectral Doppler should be part of every carotid ultrasound exam. It provides important hemodynamic information and is indispensible for the quantification of stenosis. Measurements should only be performed in a longitudinal view. As a minimal requirement spectral Doppler tracings should be obtained at the following locations:
- Distal common carotid artery (dist. CCA)
- Proximal internal carotid artery (prox. ICA)
- Proximal external carotid artery (prox. ECA)
- Vertebral artery
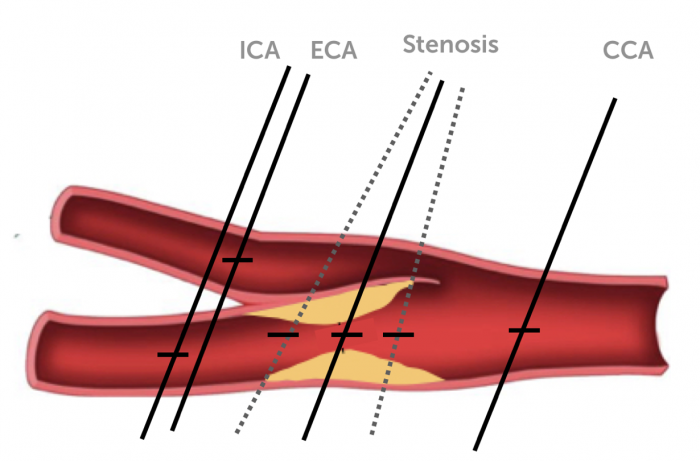 lacement Doppler: location where the sample volume should be placed (minimal protocol) Multiple measurements should be performed at the location of a stenosis to detect the highest velocity
lacement Doppler: location where the sample volume should be placed (minimal protocol) Multiple measurements should be performed at the location of a stenosis to detect the highest velocity
When using an extended protocol additional measurements can be recorded at:
- Proximal common carotid artery (prox. CCA)
- Mid common carotid artery (mid CCA)
- Mid internal carotid artery (mid ICA)
- Distal internal carotid artery (dist ICA)
In the presence of a stenosis multiple measurements should be performed at the location of the stenosis in an attempt to record the highest velocities but, also immediately before and after the stenosis. Be aware that the flow direction does not necessarily follow the orientation of the vessel in the presence of a stenosis.
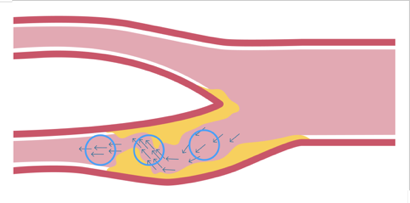 Direction of flow in stenosis: It is important to consider the direction of flow when performing Spectral Doppler measurements at stenotic lesions (the direction of flow does not always follow the lumen of the vessel in stenosis)
Direction of flow in stenosis: It is important to consider the direction of flow when performing Spectral Doppler measurements at stenotic lesions (the direction of flow does not always follow the lumen of the vessel in stenosis)
12.2 Which parameters should be obtained from the spectral Doppler Tracing?
For the quantification of carotid artery stenosis measure both the peak systolic as well as the end diastolic velocity. These velocities will be elevated in the presence of a relevant stenosis. Measurements can be performed manually or with automatic tracing / measurement features.
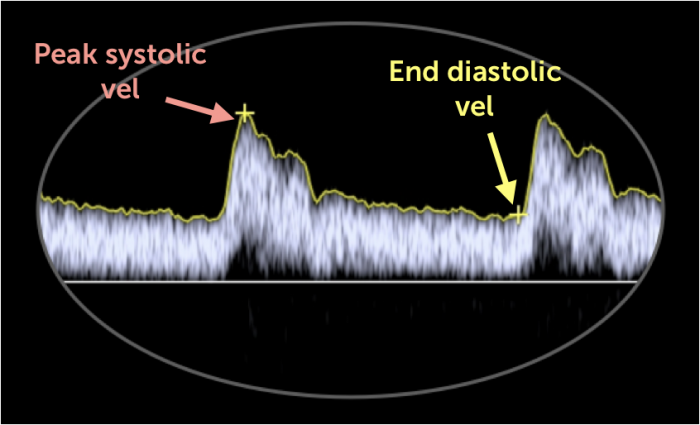 Where to measure curve: doppler tracing recorded in the proximal internal carotid artery (ICA) in a normal individual. The (+) denotes the point of measurements for the peak systolic (pink) and end-diastolic (yellow) velocities.
Where to measure curve: doppler tracing recorded in the proximal internal carotid artery (ICA) in a normal individual. The (+) denotes the point of measurements for the peak systolic (pink) and end-diastolic (yellow) velocities.
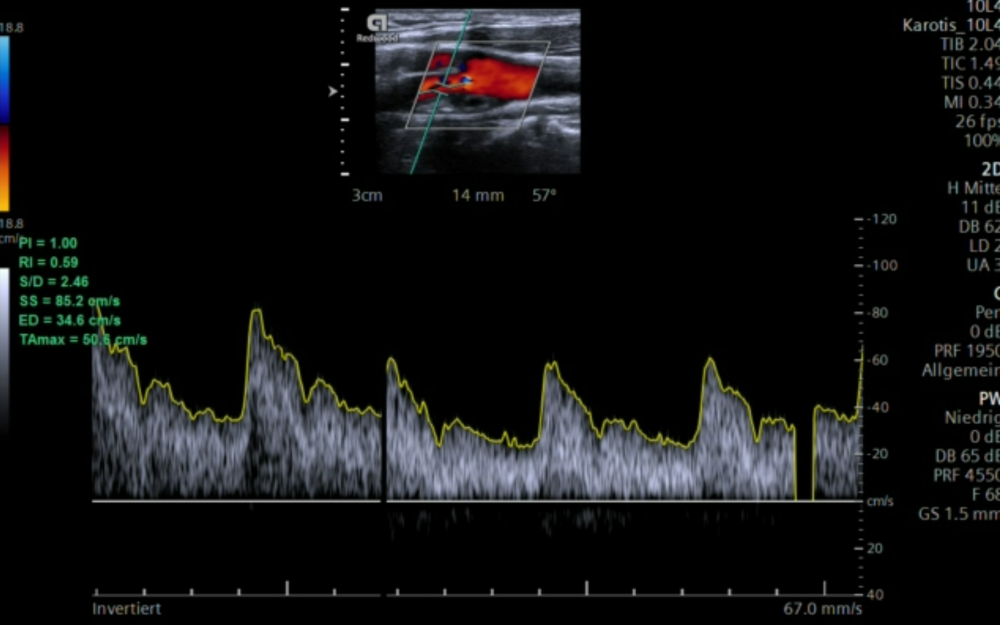 Doppler velocity rise: positioning of the sample volume into the region with the greatest lumen reduction causes a sudden rise of the Doppler velocities.
Doppler velocity rise: positioning of the sample volume into the region with the greatest lumen reduction causes a sudden rise of the Doppler velocities.
12.3 Which ratios should be calculated
It is important to also calculate velocity ratios. Especially the peak systolic velocity index, which is the ratio between the peak systolic velocity in the ICA vs. the CCA (PSV). In contrast to absolute velocity values of peak systolic and diastolic velocities, ratios are not affected by hypo- or hyperdymamic circulatory states (i.e. hyperdynamic left ventricular function). Ratios are also helpful in the presence of contralateral occlusion. Most scanners provide measurement programs or computer based spectral Doppler tracing algorithms where the ratios are automatically calculated.
Spectral Doppler Ratios
Parameter Formula MV Mean velocity MV = PSV + 2 EDV / 3 PI Pulsatility Index (Pourcelot) PI = PSV - EDV / MV RI Resistance Index (RI) RI = PSV - EDV / PSV PSI Peak systolic Index PSI = PSVICA/ PSVCCA DI Diastolic Index DI = EDVICA / EDVCCA SMR St. Mary Ratio SMR = PSVICA / EDVCCASpectral Doppler facts and tips
- Peak systolic velocity is the main parameter used to quantify a stenosis
- Diastolic velocities increase in the internal carotid artery in the presence of a stenosis
- Diastolic velocities decreases in the common carotid artery (CCA) if a stenosis is present in the internal carotid artery because the resistance to flow increases.
- You will see spectral broadening of the signal in stenosis (but also in tortuous vessels)
- Angle correction: the Doppler angle of insonation should be ≤60°
- Measure peak systolic and peak diastolic velocities / calculate ratios
- Don’t use ectopic and post ectopic beats. - Average several beats in atrial fibrillation
- Use automatic measurements only if Doppler quality is good, avoid artefacts
12.4 How can you grade a stenosis of the internal carotid artery based on spectral Doppler?
Doppler based quantification of carotid artery stenosis is widly accepted as the most reliable method. Several grading schemes have been proposed, which vary somewhat with respect to the cutoff values. In general peak systolic velocity that exceeds 125cm/s and a PSV ratio of more than 2 denotes the presence of a stenosis of more than 50%. Very severe severe stenosis (<90) is present if the maximal systolic velocity exceeds 400cm/a and the PSV index is >5.
Note: In near occlusion the flow velocities will drop (trickle flow)
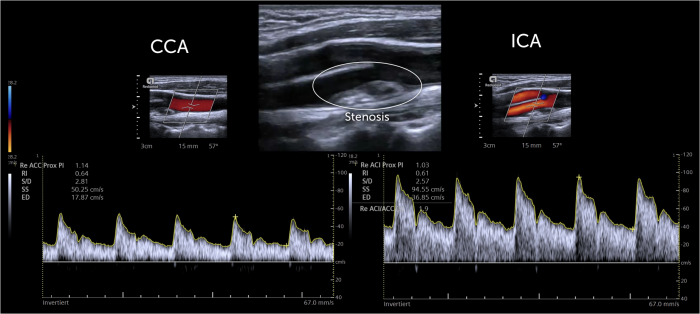
 Example Doppler Severe. Example of a patient with severe (80-90%) right internal carotid artery stenosis. The maximal peak systolic (PS) velocity is 366 cm/s, the PSV index is 6.5 and the St. Mary Index is 26
Example Doppler Severe. Example of a patient with severe (80-90%) right internal carotid artery stenosis. The maximal peak systolic (PS) velocity is 366 cm/s, the PSV index is 6.5 and the St. Mary Index is 26
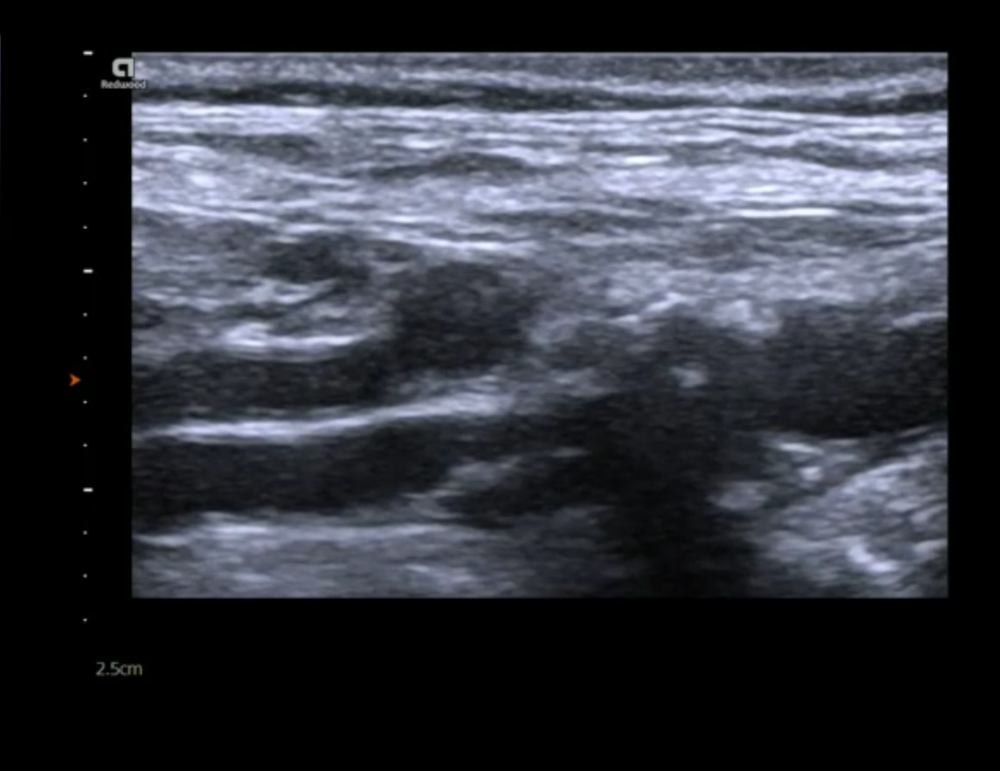
 Mild Carotid stenosis. Large plaque with mild (
Mild Carotid stenosis. Large plaque with mild (
Stenos - grading scheme ICA
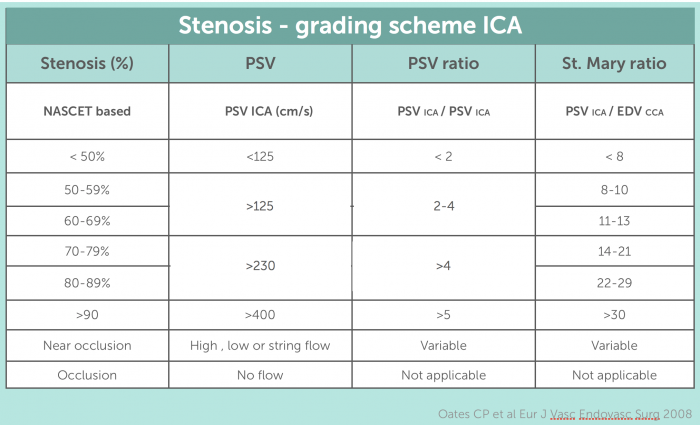 Table Grading Scheme ICA Stenosis Grading scheme for the quantification of internal carotid artery stenosis (ICA). Comparison of the NASCET based quantification with the peak systolic velocity, the peak systolic velocity ratio/index and the St. Mary ratio.
Table Grading Scheme ICA Stenosis Grading scheme for the quantification of internal carotid artery stenosis (ICA). Comparison of the NASCET based quantification with the peak systolic velocity, the peak systolic velocity ratio/index and the St. Mary ratio.
With an increase of stenosis we not only see an increase in the systolic velocity but also of diastolic velocities. The following table provides a grading scheme based on diastolic velocities, which can be used in conjunction with the above-mentioned systolic parameters and ratios.
Grading scheme for ICA stenosis based on diastolic velocities
Stenosis (%) ICA EDV < 50% < 40cm/s 50-69 % > 40 - 100cm/s >70% >100cm/2
12.5 How do you grade common carotid artery stenosis?
Both ratios and peak velocities are also used for the quantification of common carotid artery (CCA) stenosis. One should determine the highest velocity in the stenosis and also measure proximal and distal to the stenosis to calculate the CCA ratio. The following table provides a quantification scheme.
Grading scheme common carotid artery stenosis
Stenosis (%) CCA ratio (max systolic vel post/pre stenosis) 0-49% <2 50-74 % ≥ 2 75-99% ≥4 occluded no flow
12.6 How do you grade external carotid artery stenosis?
Stenosis of the external carotid artery is not uncommon but quantification is usually not as critical since patients are rarely symptomatic and are not at risk of an ischemic event from an external carotid artery stenosis. The external carotid artery however, can provide collaterals in the setting of an ipsilateral carotid artery stenosis or occlusion. The external carotid artery can also be involved in the presence of plaque of the bifurcation, which involves both vessels (ECA and ICA). A stenotic lesion of the external carotid artery should also be described in the report.
The following table provides a grading scheme for external carotid artery (ECA) stenosis.
Grading scheme external carotid artery stenosis
Stenosis (%) If ipsilateral < 70% ICA stenosis If ipsilateral > 70% ICA stenosis ≥50% 130cm/s ≥ 190cm/s ≥ 75 220cm/s ≥ 200 cm/s occluded no flow no flow
12.7 Which factors influence the velocity in the arteries?
Velocities in the arteries can vary greatly from one individual to another. When assessing flow and quantifying the degree of stenosis it is important to know the potential causes for these variations.
Factors which influence velocites (pitfalls)
Problem Cause Effect Vessel size Large or small vessels, Lower velocity in larger vessels Vessel geometry Aneurysms, shape of the bifurcation Variable effects Age / blood pressure Hyper and hypotension Velocity decreases with age, hypertension can increases velocities Contralateral occlusion Collateral flow Increased velocities in the contralateral artery Low cardiac output Heart failure, low flow aortic stenosis, cardiomyopathies Decrease in velocity High cardiac output Anxiety, toxic drugs, medication, hyperthyroidism Increases velocity Beat to beat variations Atrial fibrillation, ectopic beats Increase velocities (post ES beat or long RR interval) Aortic regurgitation Aortic valve dysfunction acute or chronic Diastolic retrograde flow may influence diastolic parameters (i.e. St. Mary's index)
12.8 How do you deal with calcified lesions?
Calcified lesions are more difficult to assess then lesions, which are formed by soft plaque. Acoustic shadowing causes dropouts in both the B mode image and Color Doppler. The quality of the spectral Doppler tracing can also be affected.
 Calcified Loop: example of a heavily calcified bifurcation and proximal internal carotid artery (ICA)
Calcified Loop: example of a heavily calcified bifurcation and proximal internal carotid artery (ICA)
- The following table provides some tips on how to assess patients with calcified lesions.
- Use multiple planes to avoid / reduce shadowing
- Use transverse view to check if the calcified plaque is circumferential (this makes it more difficult to quantify stenosis!)
- Look at aliasing / velocity distal to the stenosis. If there is no color flow aliasing or increased velocity then a significant stenosis is unlikely
- A low PSV/EDV ratio distal to the plaque indicates a relevant stenosis
- If a calcified lesion is long (>1cm) then it is not possible to exclude a hemodynamically relevant stenosis - you will need CT or MRI angio
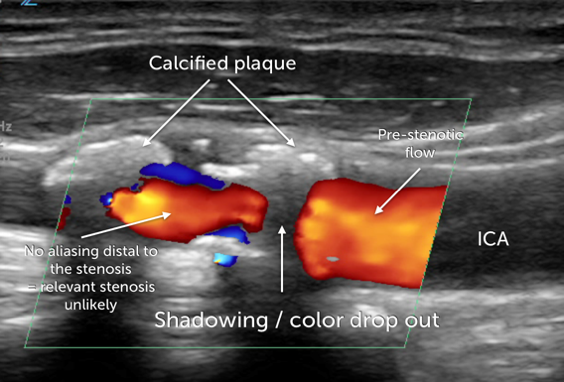 Calcified lesion illustr. Example of a heavily calcified lesion of the internal carotid artery which causes acoustic shadowing. However, absence of turbulent flow distal to the stenosis excludes severe stenosis
Calcified lesion illustr. Example of a heavily calcified lesion of the internal carotid artery which causes acoustic shadowing. However, absence of turbulent flow distal to the stenosis excludes severe stenosis
12.9 How can I detect carotid artery occlusion?
Carotid artery occlusion can be difficult to diagnose. The echogenicity of the occluded lumen is increased and may be difficult to discern from the surrounding tissue. Sometimes you will see a “to-and-fro” motion of the artery. You will only find a weak (trickle flow) or even no Doppler signal (Color and spectral Doppler) The velocities will be low proximal to the occlusion. Flow velocities will be higher in the contralateral CCA. If the ipsilateral CCA is occluded without involvement of the ICA you might be able to see retrograde flow (collateral flow) from the external carotid artery via the bifurcation into the ICA.
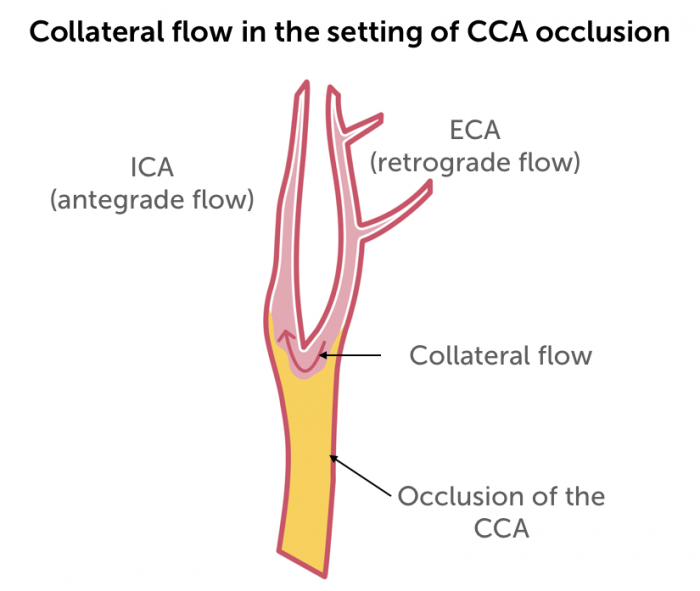 Occlusion of the common carotid artery with collateral flow via the external carotid artery
Occlusion of the common carotid artery with collateral flow via the external carotid artery
.pagination .pager .pager__item { font-size: 12px; } .pagination .pager .pager__item--current { padding: initial; } .pagination { margin: 0; margin: 0 auto; margin-top: 0 !important; } .pager { margin-top: 0 !important; padding: 0; display: flex; } .pagination .pager { padding: 0; } .pagination .pager a { padding: 8px 12px; } .pager__item a { box-shadow: none !important; } .aut-nav-carotid-p { text-align: center !important; margin-bottom: 6px !important; } function advagg_mod_2() { // Count how many times this function is called. advagg_mod_2.count = ++advagg_mod_2.count || 1; try { if (advagg_mod_2.count <= 40) { var autNaviCarotid1 = ('\ \
- \
- \
Chapters\
\
- \ 1\ \
- \ 2\ \
- \ 3\ \
- \ 4\ \
- \ 5\ \
- \ 6\ \
- \ 7\ \
- \ 8\ \
- \ 9\ \
- \ 10\ \
- \ 11\ \
- \ 12\ \
- \ 13\ \
- \ 14\ \
- \ 15\ \
- \ last »\ \ \ \ '); var autNaviCarotid2 = ('\
Carotid Ultrasound Webbook & Wiki\ \
- \
- \
‹ previous\
\
- \ BACK TO OVERVIEW\ \
- \ next ›\ \ \ \ '); (function($) { $(document).ready(function(){ $(".sonopl-article.sonopl-book__content.sonopl-content-main") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); $(".aut-nav-carotid") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); }); }(jQuery)); // Set this to 100 so that this function only runs once. advagg_mod_2.count = 100; } } catch(e) { if (advagg_mod_2.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_2, 250); } } } function advagg_mod_2_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_2(); } else { window.setTimeout(advagg_mod_2_check, 250); } } advagg_mod_2_check();
If you like the way we teach, please leave a message!
- \ BACK TO OVERVIEW\ \
- \ 1\ \


