4. B mode imaging – Carotid artery
/* .lity-iframe-container iframe { background: #fff !important; } */ .articles__categories nav { display: none !important; } .sonopl-book__aside .articles__categories { background: #f5f5f5; } .sonopl-article th, .sonopl-article td { color: black; text-align: left; } function advagg_mod_1() { // Count how many times this function is called. advagg_mod_1.count = ++advagg_mod_1.count || 1; try { if (advagg_mod_1.count <= 40) { var getClass = document.querySelectorAll(".articles__categories"); var a = document.createElement('a'); var linkText = document.createTextNode("Get Carotid MC Free Lectures"); a.appendChild(linkText); a.title = "newsletter"; a.href = "/overlay/forms/cu_mc/16618"; a.setAttribute("class", "sonopl-button sonopl-button--default"); a.setAttribute("data-lity", ""); a.style = "line-height: 1.2;margin-top: 25px;padding: 15px;width: 100%;"; for(var ix = 0; ix < getClass.length; ix++) { getClass[ix].appendChild(a) } // Set this to 100 so that this function only runs once. advagg_mod_1.count = 100; } } catch(e) { if (advagg_mod_1.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_1, 250); } } } function advagg_mod_1_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_1(); } else { window.setTimeout(advagg_mod_1_check, 250); } } advagg_mod_1_check();
4.0 How should you image the carotid and vertebral arteries?
The carotid artery is not very difficult to image. However, to obtain good image quality it is very important to follow certain rules. Don’t forget: the carotid artery is usually only 1 cm in width, and its branches are even samller. Therefore you will need very subtle motions to obtain optimal results. The angle of insonation and scanner settings are equally important to allow you to see structures with little echogenicity such as soft plaques.
4.1 From where should I scan the carotid artery?
There are several approaches to scanning the vessels of the neck:
- The observer is positioned on the right of the patient. Imaging is performed with the right.
- The observer is positioned to the left of the patient. Imaging is performed with the left hand and the scanner is operated with the right hand
- The observer is positioned at the head of the patient. Scanning is performed with the left hand and the scanner is operated with the right hand
- The observer is positioned at the head of the patient. Scanning is performed with the right hand and the scanner is operated with the left hand
Positioning of the observer on the side of the patient is usually the preferred method of operators who also perform echocardiography or abdominal scanning as the ultrasound scanner does not need to be moved to perform a carotid scan. Some operators also prefer to switch the scanning hand depending on which side of the neck (left or right) they are scanning. The bottom line: There is no "wrong" or "right" approach
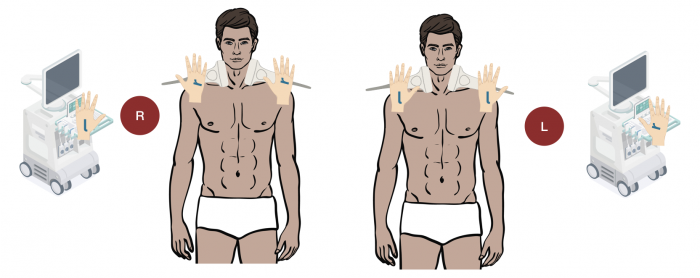 Scanning positions for carotid ultrasound. The operator is positioned either on the left or the right of the patient.
Scanning positions for carotid ultrasound. The operator is positioned either on the left or the right of the patient.
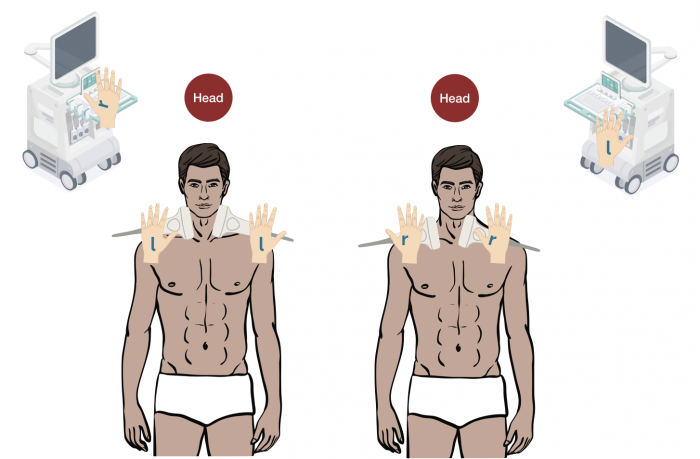 Scanning positions for carotid ultrasound. The operator is positioned at the head of the patient and images either with the left or the right hand.
Scanning positions for carotid ultrasound. The operator is positioned at the head of the patient and images either with the left or the right hand.
4. 2 How can the transducer be manipulated?
There are 3 ways how the transducer can be manipulated: Tilting, rotation and sliding. To obtain optimal images it is important to combine these there motions. Tilting is especially important to optimize the angle of insonation. Rotation is used to move from a longitudinal into a transverse view. Sliding is applied to move the transducer medial-lateral or cranial-caudal.
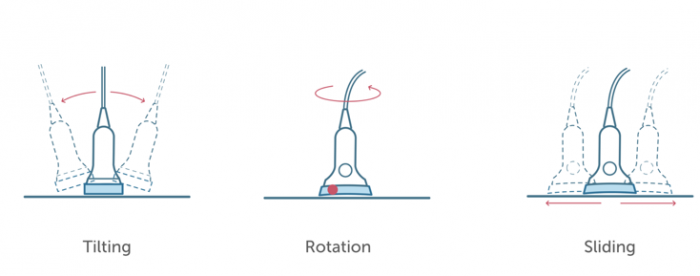 Transducer motion. This illustration demonstrates how the transducer can be manipulated for carotid ultrasound.
Transducer motion. This illustration demonstrates how the transducer can be manipulated for carotid ultrasound.
There are two main image orientations: Longitudinal (caudal – cranial orientation) and transverse (medial-lateral, anterior-posterior). Beware that the carotid arteries can also be tortuous. This is why the orientation of the transducer relative to the neck does not always correlate with the orientation of the carotid artery on the image. To display the carotid artery on a longitudinal or transverse view it is sometimes necessary to perform “oblique” views.
4.3 Which transducer orientations and views should we use for carotid ultrasound?
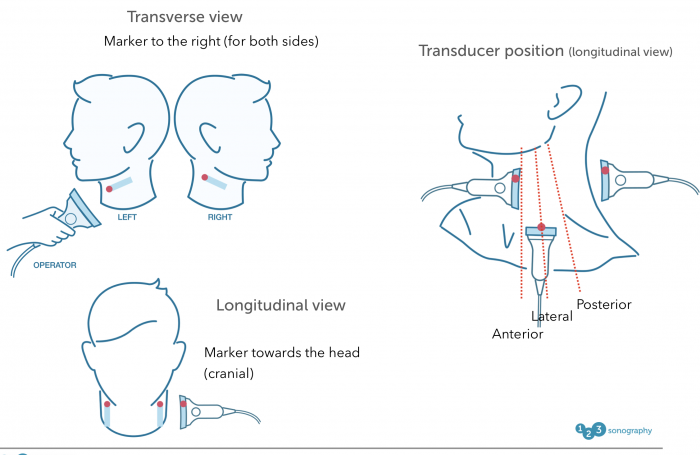 Transducer orientation: Top left: transverse image orientation. The marker (red) is always points to the left of the patient. Bottom left: Longitudinal orientation. The marker points to the head of the patient. Right: imaging in a longitudinal orientation can be performed anterior, lateral or posterior
Transducer orientation: Top left: transverse image orientation. The marker (red) is always points to the left of the patient. Bottom left: Longitudinal orientation. The marker points to the head of the patient. Right: imaging in a longitudinal orientation can be performed anterior, lateral or posterior
4.4 What are the advantages and disadvantages of the individual views?
A standard carotid ultrasound exam should always incorporate transverse and longitudinal views from various positions (cranial-caudal, anterior, lateral and posterior) in both B mode and using color and spectral Doppler. The following table demonstrates the individual application of the transverse and longitudinal view.
Transverse Longitudinal Gives good overview of the vessels Better deletion of the vessel wall Allows visualization of the entire vessel wall Allows assessment of the origin of the CCA Helps to understand the topography (ICA vs. Permits measurements of IMT Allows assessment of area reduction in stenosis Allows color Doppler assessment of flow Helps to understand the exact location of plaques Allows measurements of plaque length Helps to detect kinking Permits measurements of flow velocities (PW Doppler) Allows assessment of neck pathologies and adjacent structures Can be used to display the vertebral arteries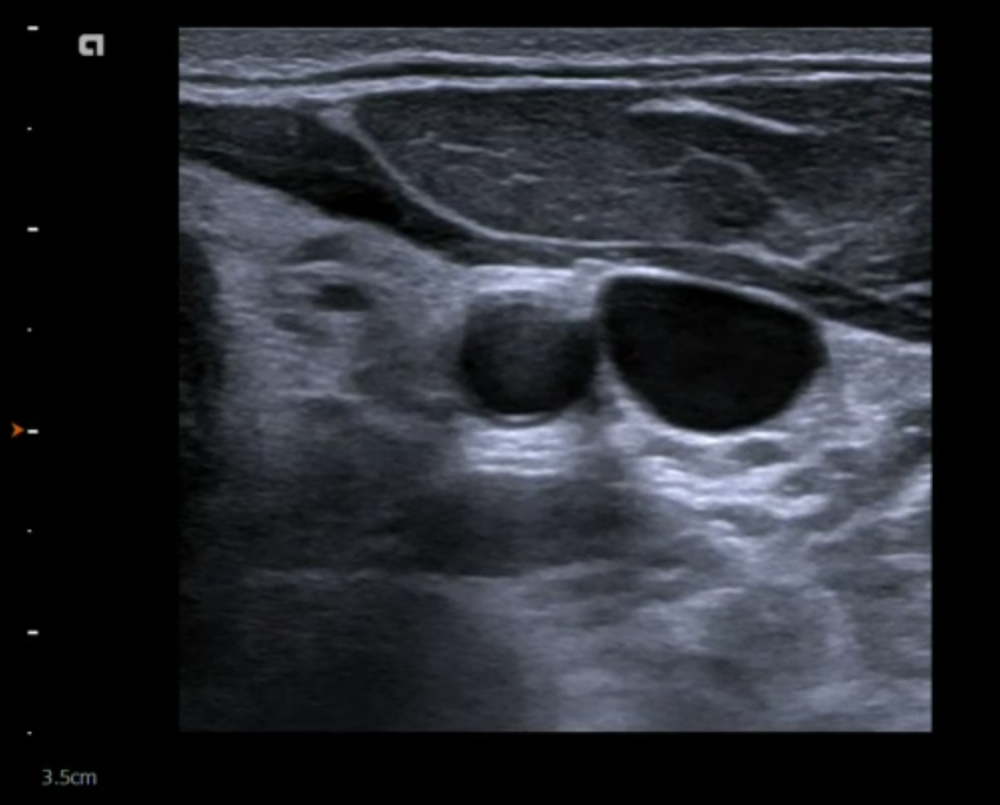 Transverse view. Typical ultrasound view of the common carotid artery (and jugular vein). Note that the jugular vein can be compressed by applying pressure on the transducer.
Transverse view. Typical ultrasound view of the common carotid artery (and jugular vein). Note that the jugular vein can be compressed by applying pressure on the transducer.
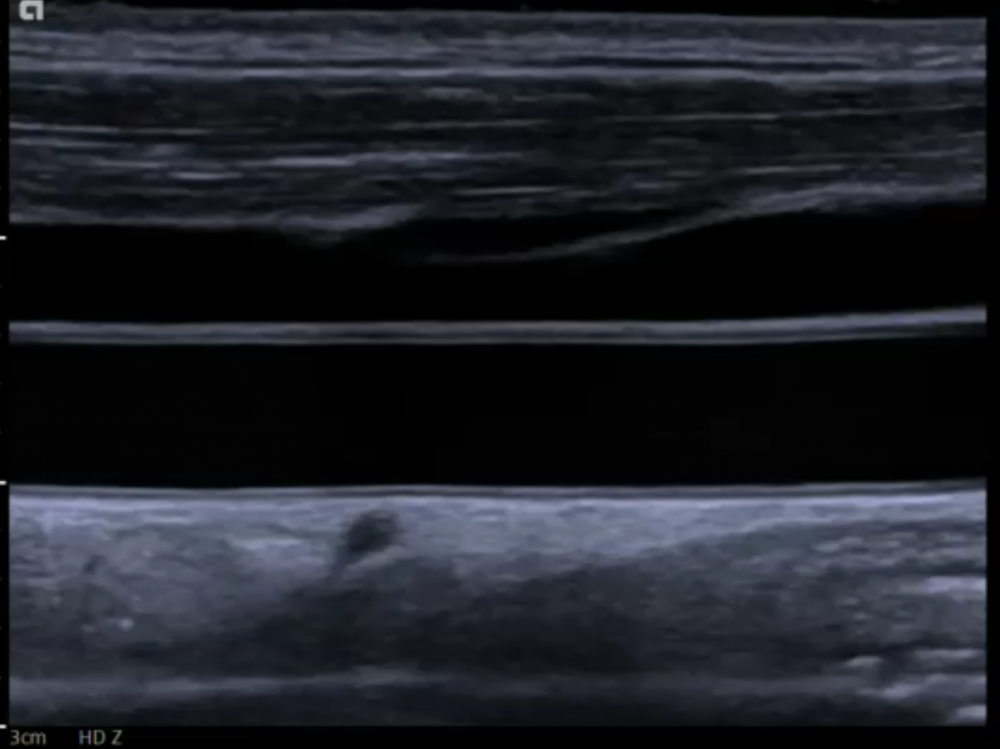 Longitudinal view. Typical ultrasound image of the common carotid artery. The jugular vein can be seen ventral to the common carotid artery
Longitudinal view. Typical ultrasound image of the common carotid artery. The jugular vein can be seen ventral to the common carotid artery
4.5 Imaging of the Bifurcation.
The bifurcation is an important region in carotid ultrasound. This is where you will find the vast majority of plaques and stenotic lesions. The bifurcation can be displayed showing both the external and the internal carotid artery in the same image (displayed as a fork) in approximately 20% of all patients. In all other patients it will be necessary to fan the transducer lateral/medial to display the internal and external artery sequentially.
Bifurcation facts / imaging tips Most common site of plaques Includes the bulb It usually originates above the superior boundary of the thyroid Large variation in appearance of the bifurcation High bifurcations are difficult to image „The fork“ display (ICA and ECA in one image) can only be achieved in approximately 10% of patients If you do not see the fork - the region where the vessel gets larger is usually the bifurcation Tilt back and forth lateral and medial to display once the ICA then the ECA Also use a transverse view to study the bifurcation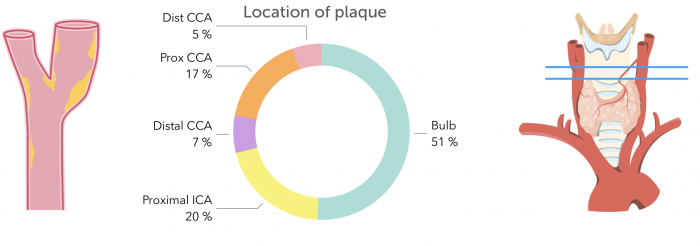 Left and middle: Typical location of atherosclerotic plaques in the carotid artery. Right: Topography of the bifurcation in relationship to the thyroid. Typically the bifurcation is cranial to the superior boarder of the thyroid
Left and middle: Typical location of atherosclerotic plaques in the carotid artery. Right: Topography of the bifurcation in relationship to the thyroid. Typically the bifurcation is cranial to the superior boarder of the thyroid
 Bifurcation normal: Ultrasound of the carotid bifurcation. The common carotid artery divides into the internal (bottom) and external carotid artery (top)
Bifurcation normal: Ultrasound of the carotid bifurcation. The common carotid artery divides into the internal (bottom) and external carotid artery (top)
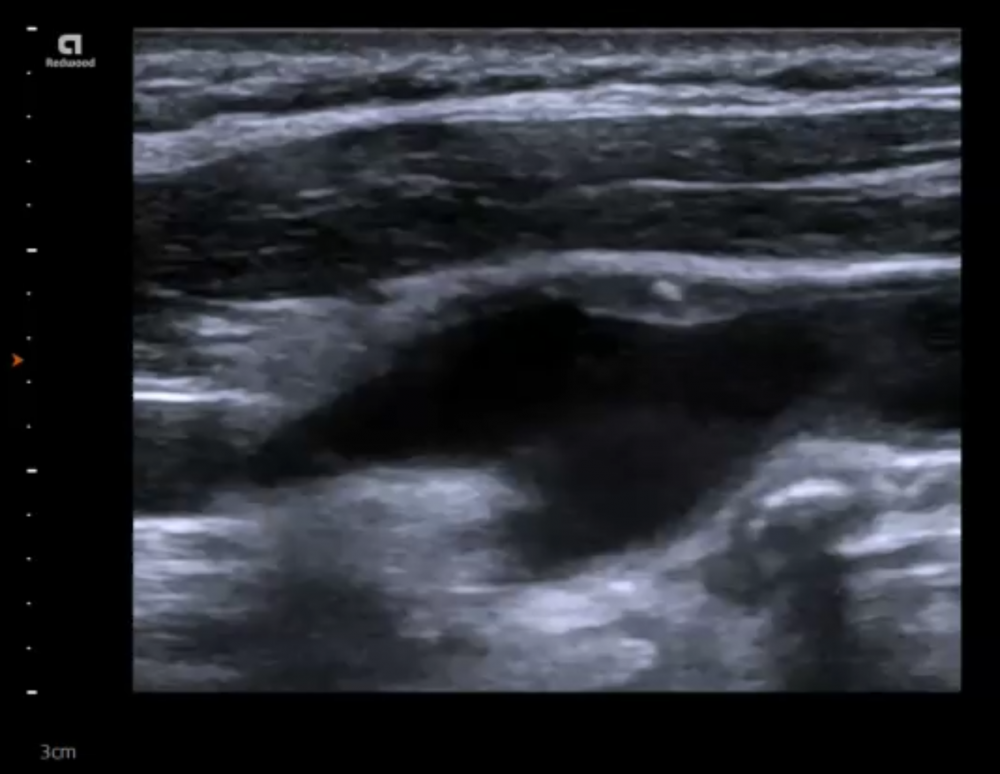 Bifurcation_Plaque: Imaging of the carotid bifurcation: The bifurcation shows mixed atherosclerotic plaque.
Bifurcation_Plaque: Imaging of the carotid bifurcation: The bifurcation shows mixed atherosclerotic plaque.
.pagination .pager .pager__item { font-size: 12px; } .pagination .pager .pager__item--current { padding: initial; } .pagination { margin: 0; margin: 0 auto; margin-top: 0 !important; } .pager { margin-top: 0 !important; padding: 0; display: flex; } .pagination .pager { padding: 0; } .pagination .pager a { padding: 8px 12px; } .pager__item a { box-shadow: none !important; } .aut-nav-carotid-p { text-align: center !important; margin-bottom: 6px !important; } function advagg_mod_2() { // Count how many times this function is called. advagg_mod_2.count = ++advagg_mod_2.count || 1; try { if (advagg_mod_2.count <= 40) { var autNaviCarotid1 = ('\ \
- \
- \
Chapters\
\
- \ 1\ \
- \ 2\ \
- \ 3\ \
- \ 4\ \
- \ 5\ \
- \ 6\ \
- \ 7\ \
- \ 8\ \
- \ 9\ \
- \ 10\ \
- \ 11\ \
- \ 12\ \
- \ 13\ \
- \ 14\ \
- \ 15\ \
- \ last »\ \ \ \ '); var autNaviCarotid2 = ('\
Carotid Ultrasound Webbook & Wiki\ \
- \
- \
‹ previous\
\
- \ BACK TO OVERVIEW\ \
- \ next ›\ \ \ \ '); (function($) { $(document).ready(function(){ $(".sonopl-article.sonopl-book__content.sonopl-content-main") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); $(".aut-nav-carotid") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); }); }(jQuery)); // Set this to 100 so that this function only runs once. advagg_mod_2.count = 100; } } catch(e) { if (advagg_mod_2.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_2, 250); } } } function advagg_mod_2_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_2(); } else { window.setTimeout(advagg_mod_2_check, 250); } } advagg_mod_2_check();
If you like the way we teach, please leave a message!
- \ BACK TO OVERVIEW\ \
- \ 1\ \


