16.2.2.3 Indirect signs of pulmonary hypertension
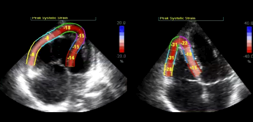
The 2D image of the heart in severe pulmonary hypertension is so characteristic that it rarely poses a problem in terms of diagnosis. The most prominent features of severe pulmonary hypertension are dilatation of the right ventricle and systolic "flattening" of the interventricular septum. Flattening of the IVS is the result of high pressure in the right ventricle, which exceeds that of the left ventricle during systole. As a result the septum is shifted towards the left ventricle, which is then eccentric and D-shaped. The degree of eccentricity (eccentricity index) is measured by dividing the longest diameter by the shortest one in a short axis at the level of the papillary muscles. This yields the eccentricity index, which actually correlates with the degree of pulmonary hypertension. However, the degree of flattening also depends on systolic pressure in the left ventricle. Thus, in the setting of systemic arterial hypertension there may be no or mild flattening despite high pulmonary pressures.
When a patient has additional (moderate to severe) tricuspid regurgitation, right ventricular volume overload will result in flattening during diastole as well. Hence a D-shaped ventricle will be present during systole as well as diastole.
As a result of right ventricular dilatation and the shift of the interventricular septum to the left, the left ventricle is usually rather small and slim. The distorted geometry of the left ventricle also affects filling and contraction of the left ventricle. Compression of the mitral valve annulus may result in a "pseudoprolapse" of the mitral valve. However, in contrast to classic mitral valve prolapse, the valve is not thickened and significant mitral regurgitation is almost never present.
Right ventricular hypertrophy is also a consistent finding. This is best appreciated in an atypical four-chamber view which displays the free lateral wall of the right ventricle as well as in subcostal views. The thickness of the right ventricular wall may be far in excess of 5 mm and is sometimes identical to the wall thickness of the left ventricle.
In contrast to the left ventricle, the right is much more sensitive to an increase in afterload. Therefore one will frequently see a reduction in right ventricular function. Practically all patients with moderate/severe pulmonary hypertension will have some degree of right ventricular contractile dysfunction. The degree of RV dysfunction also correlates with symptoms and prognosis. The main problem in clinical practice is the difficulty to quantify the degree of right ventricular dysfunction. All of the available quantification techniques (see Chapter 3, Heart Chambers and Walls) have their limitations. It becomes especially difficult to assess right ventricular function in the presence of additional tricuspid regurgitation: right ventricular function might appear better than it actually is because tricuspid regurgitation results in a reduction of afterload.
Pulmonary hypertension also causes dilatation of the pulmonary artery and its branches. The pulmonary artery becomes larger than the aorta. Its diameter may exceed 25 mm. In some patients the pulmonary artery may become so large that it may be prone to rupture. Dilatation of the pulmonary annulus may also increase the degree of pulmonary regurgitation. However, severe pulmonary regurgitation is a rare finding.
An important finding in pulmonary hypertension is pericardial effusion. It is probably related to elevated right atrial pressure and impaired venous and lymphatic drainage, but the exact mechanism is not fully understood. Pericardial effusion is usually mild and never causes tamponade. Thus, a pericardial tap is not required. However, its presence is correlated with the severity of pulmonary hypertension and signifies a poor prognosis.