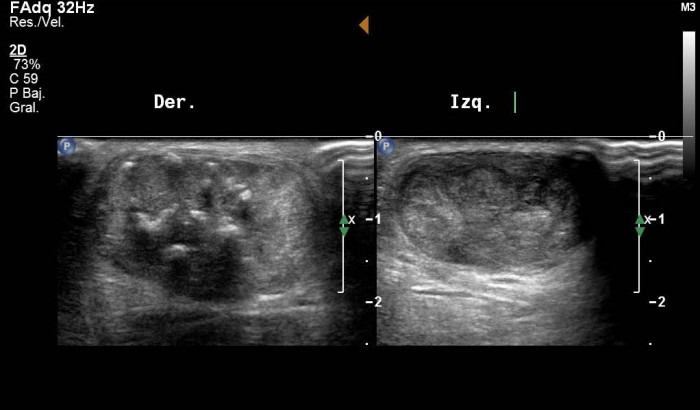
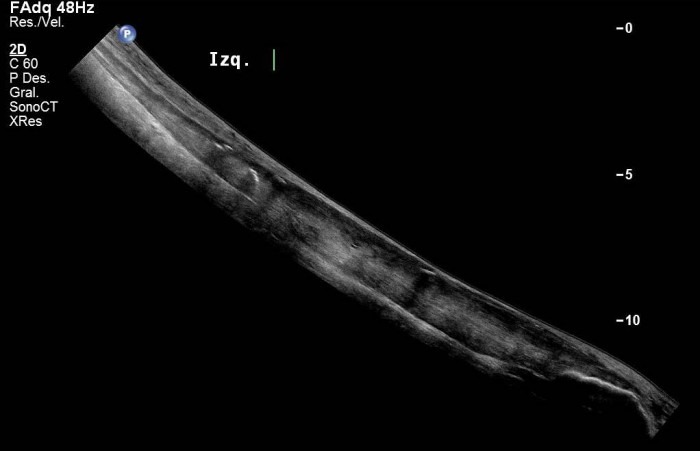
Bilateral Achilles Tendinosis
First published on SonoWorld
Case Presentation
75 year old male patient. The posterior region of distal segment of both legs were painful and swollen.


Differential Diagnosis
- Bilateral Achilles Tendinosis
- Rupture of Achilles Tendon
Final Diagnosis
Bilateral Achilles Tendinosis
Discussion
Tendinosis is a chronic condition due to degenerative tendinopathy. It usually occurs in patients who are between 35 and 45, and who are not necessarily athletic. The Achilles tendon is swollen and thickened.
Ultrasonography is an excellent method for the diagnosis of acute and chronic Achilles tendon disorders. By using sonography it is possible to detect many conditions that affect this tendon such as peritendinous edema, bursitis, ruptures of the Achilles tendon, and calcified insertion of the tendon at the calcaneous.
B mode ultrasonographic findings in Achilles tendinosis may include:
enlargement (AP >6 mm) usually presenting as localized fusiform enlargement
disruption of the normal fibrillar striation pattern of the tendon
intratendinous hypoechoic areas due to chronic mucoid degeneration
extra-tendinous hypoechoic areas due to edema
focal calcifications
Color Doppler may show increased flow in the intra and extra-tendinous regions, depending on the grade of inflammation present; the higher the grade, the more Doppler signal can be observed.
Follow Up
Ultrasound findings confirmed the initial clinical diagnosis of bilateral Achilles tendinosis. The patient was referred for shock-wave (orthotripsia) treatment and physical therapy.
Technical Details
Philips iU22 ultrasound system with a L17-5 (17 to 5 Mhz) linear transducer.
Grechenig W et al. Ultrasound diagnosis of the Achilles tendon. Orthopade. 2002; 31(3):319-25
Koenig MJ et al. Preliminary results of colour Doppler-guided intratendinous glucocorticoid injection for Achilles tendonitis in five patients. Scand J Med Sci Sports. 2004; 14(2):100-6